Drug Information
Drug (ID: DG00038) and It's Reported Resistant Information
| Name |
Erythromycin
|
||||
|---|---|---|---|---|---|
| Synonyms |
Abboticin; Abomacetin; Acneryne; Acnesol; Aknemycin; Aknin; AustriaS; Benzamycin; Derimer; Deripil; Dotycin; Dumotrycin; ERY; ERYC; Emgel; Emuvin; Emycin; Endoeritrin; Erecin; Erisone; Eritomicina; Eritrocina; Eritromicina; Ermycin; Eros; Eryacne; Eryacnen; Erycen; Erycette; Erycin; Erycinum; Eryderm; Erydermer; Erygel; Eryhexal; Erymax; Erymed; Erysafe; Erytab; Erythro; Erythroderm; Erythrogran; Erythroguent; Erythromid; Erythromycine; Erythromycinum; Erytop; Erytrociclin; Ilocaps; Iloticina; Ilotycin; Inderm; IndermRetcin; Latotryd; Lederpax; Mephamycin; Mercina; Oftamolets; Paediathrocin; Pantoderm; Pantodrin; Pantomicina; Pharyngocin; Primacine; Propiocine; Proterytrin; Retcin; Robimycin; Romycin; Sansac; Staticin; Stiemicyn; Stiemycin; Tiloryth; Tiprocin; Torlamicina; Wemid; Akne Cordes Losung; Aknederm Ery Gel; Benzamycin Pak; ERYTHROMYCIN STEARATE; Eryc Sprinkles; Erythromycin A; Erythromycin Lactate; Erythromycin Ointment; Erythromycin base; Erythromycin intravenous; Erythromycin sodium lauryl sulfate; Inderm Gel; Oftalmolosa Cusi Eritromicina; Skid Gel E; Theramycin Z; Udima Ery Gel; E0751; Eryc 125; Erythromast 36; Ak-Mycin; Akne-Mycin; Del-Mycin; E-Base; E-Glades; E-Mycin; E-Solve 2; ERYC (base); Emu-V; Emu-Ve; Erimycin-T; Eritromicina [INN-Spanish]; Ery-B; Ery-Diolan; Ery-Sol; Ery-Tab; Ery-maxin; Eryc (TN); Eryc-125; Eryc-250; Erygel (TN); Erythra-Derm; Erythro-Statin; Erythro-Teva; Erythromycin & VRC3375; Erythromycine [INN-French]; Erythromycinum [INN-Latin]; Ilosone (TN); Ilosone (estolate); Ilotycin T.S; Kesso-Mycin; N-Methylerythromycin A; PCE Dispertab (base); Pce (TN); R-P Mycin; Sans-acne; Staticin (TN); T-Stat; Taimoxin-F; A/T/S; Akne-mycin (TN); C-Solve-2; E-Base (base); E-Mycin (base); Ery-Tab (base); Erythromycin [INN:BAN:JAN]; Ilotycin T.S.; T-stat (TN); E-mycin, Erycin, Robimysin; Erythromycin (JP15/USP/INN); Erythromycin, compd. with monododecyl sulfate, sodium salt; Sulfuric acid, monododecyl ester, sodium salt, compd. with erythromycin; Adecane-2,10-dione (non-preferred name); Erythromycin A, T-Stat, Pantomicina, HSDB 3074, Erytab, DRG-0279; Ery
Click to Show/Hide
|
||||
| Indication |
In total 1 Indication(s)
|
||||
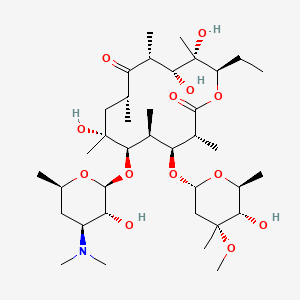
| Structure |
|
||||
| Drug Resistance Disease(s) |
Disease(s) with Clinically Reported Resistance for This Drug
(18 diseases)
[6]
[7]
[8]
[11]
[8]
[13]
[14]
[8]
[15]
[16]
[17]
[18]
[19]
[20]
[21]
[8]
[22]
Disease(s) with Resistance Information Discovered by Cell Line Test for This Drug
(1 diseases)
[12]
Disease(s) with Resistance Information Validated by in-vivo Model for This Drug
(5 diseases)
[23]
[24]
[25]
[26]
[27]
|
||||
| Target | Bacterial 50S ribosomal RNA (Bact 50S rRNA) | NOUNIPROTAC | [1] | ||
| Click to Show/Hide the Molecular Information and External Link(s) of This Drug | |||||
| Formula |
C37H67NO13
|
||||
| IsoSMILES |
CC[C@@H]1[C@@]([C@@H]([C@H](C(=O)[C@@H](C[C@@]([C@@H]([C@H]([C@@H]([C@H](C(=O)O1)C)O[C@H]2C[C@@]([C@H]([C@@H](O2)C)O)(C)OC)C)O[C@H]3[C@@H]([C@H](C[C@H](O3)C)N(C)C)O)(C)O)C)C)O)(C)O
|
||||
| InChI |
1S/C37H67NO13/c1-14-25-37(10,45)30(41)20(4)27(39)18(2)16-35(8,44)32(51-34-28(40)24(38(11)12)15-19(3)47-34)21(5)29(22(6)33(43)49-25)50-26-17-36(9,46-13)31(42)23(7)48-26/h18-26,28-32,34,40-42,44-45H,14-17H2,1-13H3/t18-,19-,20+,21+,22-,23+,24+,25-,26+,28-,29+,30-,31+,32-,34+,35-,36-,37-/m1/s1
|
||||
| InChIKey |
ULGZDMOVFRHVEP-RWJQBGPGSA-N
|
||||
| PubChem CID | |||||
| ChEBI ID | |||||
| TTD Drug ID | |||||
| VARIDT ID | |||||
| DrugBank ID | |||||
Type(s) of Resistant Mechanism of This Drug
Drug Resistance Data Categorized by Their Corresponding Diseases
ICD-01: Infectious/parasitic diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: rRNA adenine N-6-methyltransferase ermE (ERME) | [1], [2], [3] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli AS19 | 562 | ||
| Escherichia coli AS19-RrmA- | 562 | |||
| Escherichia coli DH10B | 316385 | |||
| Escherichia coli JC7623 | 562 | |||
| Experiment for Drug Resistance |
Agar dilution method assay | |||
| Mechanism Description | Methylation of specific nucleotides in rRNA is one of the means by which bacteria achieve resistance to macrolides-lincosamides-streptogramin B (MLSB) and ketolide antibiotics.ErmE dimethylation confers high resistance to all the MLSB and ketolide drugs. | |||
| Key Molecule: 23S ribosomal RNA methyltransferase Erm36 (ERM36) | [28] | |||
| Resistant Disease | Micrococcus luteus infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Micrococcus luteus MAW843 | 1270 | ||
| Experiment for Molecule Alteration |
Sequence analysis | |||
| Experiment for Drug Resistance |
Agar diffusion test assay | |||
| Mechanism Description | Erm(36) was most related (about 52-54% identity) to erythromycin-resistance proteins found in high-G+C Gram-positive bacteria and lead to drug resistance. | |||
| Key Molecule: erm(X)cj (Unclear) | [29] | |||
| Resistant Disease | Corynebacterium jeikeium infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Frameshift mutation | Codon 216 frame shift |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Corynebacterium glutamicum ATCC 13032 | 196627 | ||
| Staphylococcus aureus ATCC 29213 | 1280 | |||
| Corynebacterium diphtheriae isolate | 1717 | |||
| Corynebacterium glutamicum kO8 | 1718 | |||
| Corynebacterium jeikeium isolates | 38289 | |||
| Escherichia coli ATCC 25923 | 562 | |||
| Escherichia coli strain XL1-Blue MRF9 | 562 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Experiment for Drug Resistance |
Disk diffusion methods assay; agar dilution methods assay | |||
| Mechanism Description | Abundant amplificationproducts of slightly less than 400 bp were generated from DNAisolated from the 17 MLSb-resistant strains, whereas no am-plification products were generated with the DNA isolatedfrom the three susceptible strains. The DNA sequences of the amplification products showed 95% identity to the erm(X) gene isolated from a C. xerosis strain,erm(X)cx or ermCX. Thus, MLSb resistance in C. jeikeiumis associated with the presence of an allele, erm(X)cj, of the class Xermgenes. The first 215 amino acids of the predicted polypeptides for strains CJ12 and CJ21 are 93.5 and 98.6% identical to Erm(X)cx, the Erm protein from C. xerosi. The major difference between the two Erm(X)cj polypeptides and the Erm(X)cx polypeptide is a frame shift within codon 216. This results in the Erm(X)cj polypeptides being 31 amino acids longer than Erm(X)cx. | |||
| Key Molecule: Macrolide-lincosamide-streptogramin B resistance protein (ERMQ) | [30] | |||
| Resistant Disease | Clostridium perfringens infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli DH5alpha | 668369 | ||
| Clostridium perfringens isolates | 1502 | |||
| Escherichia coli strain JM105 | 83333 | |||
| Three MLS-resistant isolates of Clostridium difficile | 1496 | |||
| Experiment for Molecule Alteration |
Pharmacia T7 Sequencing kits assay | |||
| Mechanism Description | Erythromycin resistance among streptococci is commonly due to target site modification by an rRNA-methylating enzyme, which results in coresistance to macrolide, lincosamide, and streptogramin B antibiotics (MLSB resistance). An open reading frame with sequence similarity to erm genes from other bacteria was identified and designated the ermQ gene. On the basis of comparative sequence analysis, it was concluded that the ermQ gene represented a new Erm hybridization class, designated ErmQ. The ermQ gene therefore represents the most common erythromycin resistance determinant in C. perfringens. | |||
| Key Molecule: rRNA adenine N-6-methyltransferase ermC' (ERMC) | [31], [32], [33] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Bacillus subtilis strain BD170 | 1423 | ||
| Bacillus subtilis strain BD430 | 1423 | |||
| Bacillus subtilis strain BD431 | 1423 | |||
| Bacillus subtilis strain BD488 | 1423 | |||
| Bacillus subtilis strain BD81 | 1423 | |||
| Experiment for Molecule Alteration |
SDS-PAGE assay | |||
| Mechanism Description | The ermC gene of plasmid pE194 specifies resistance to the macrolidelincosamide-streptogramin B antibiotics. pE194 specifies an RNA methylase that can utilize either 50 S ribosomes or 23 S rRNA as substrates,with a specific dimethylation of adenine in 23 S rRNA. | |||
| Key Molecule: ErmR rRNA adenine N6-methyltransferase (ERMR) | [25] | |||
| Resistant Disease | Aeromicrobium erythreum infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Aeromicrobium erythreum strains AR18 | 2041 | ||
| Aeromicrobium erythreum strains AR1807 | 2041 | |||
| Aeromicrobium erythreum strains AR1848 | 2041 | |||
| Aeromicrobium erythreum strains AR1849 | 2041 | |||
| Aeromicrobium erythreum strains AR1850 | 2041 | |||
| Aeromicrobium erythreum strains BD170 | 2041 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Experiment for Drug Resistance |
Disk diffusion assay | |||
| Mechanism Description | Using the Ery- strain AR1807 as a recipient for plasmid-directed integrative recombination, the chromosomal ermR gene (encoding 23S rRNA methyltransferase) was disrupted, ermR-disrupted strains AR1848 and AR1849 were highly sensitive to erythromycin and the other macrolide antibiotics. Phenotypic characterizations demonstrated that ermR is the sole determinant of macrolide antibiotic resistance in A. erythreum. AR18, AR1807, and AR1850 (Ery- Ermr) were resistant to clindamycin, erythromycin, spiramycin, and tylosin (some sensitivity totylosin was observed at high concentrations). | |||
|
|
||||
| Key Molecule: Macrolide 2'-phosphotransferase II (MPHB) | [34], [35], [36] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli AG100A | 562 | ||
| Escherichia coli DB10 | 562 | |||
| Escherichia coli TOP10 | 83333 | |||
| Escherichia coli XL1-Blue | 562 | |||
| Staphylococcus aureus RN4220 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay | |||
| Experiment for Drug Resistance |
Agar dilution method assay | |||
| Mechanism Description | Mph enzymes inactivate macrolides by phosphorylating the 2'-OH of the essential dimethylamino sugar, preventing it from binding the ribosome, and providing the chemical rationale for the resistance phenotype. | |||
| Key Molecule: Oleandomycin glycosyltransferase oleD (OLED) | [6], [9], [10] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli GT-28 | 562 | ||
| Escherichia coli MurG | 562 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay | |||
| Mechanism Description | OleD displays broad acceptor specificity and hence will inactivate a wider range of macrolide antibiotics including tylosin and erythromycin. | |||
|
|
||||
| Key Molecule: ABC transporter ATPase subunit (ABCS) | [37], [38], [39] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Enterococcus faecalis isolates | 1351 | ||
| Experiment for Molecule Alteration |
Whole genome sequence assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | Multidrug efflux pump extraction, purification, and sequencing showed the distribution of mefA and msrA/msrB efflux pumps. | |||
| Key Molecule: Major facilitator superfamily efflux pump (AMVA) | [40] | |||
| Resistant Disease | Bacterial infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Acinetobacter baumannii AC0037 | 470 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | Molecular and functional characterization of a novel efflux pump, AmvA, mediating antimicrobial and disinfectant resistance in Acinetobacter baumannii. | |||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: ErmR rRNA adenine N6-methyltransferase (ERMR) | [25] | |||
| Sensitive Disease | Aeromicrobium erythreum infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Chromosome variation | Chromosome rearrangement |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Aeromicrobium erythreum strains AR18 | 2041 | ||
| Aeromicrobium erythreum strains AR1807 | 2041 | |||
| Aeromicrobium erythreum strains AR1848 | 2041 | |||
| Aeromicrobium erythreum strains AR1849 | 2041 | |||
| Aeromicrobium erythreum strains AR1850 | 2041 | |||
| Aeromicrobium erythreum strains BD170 | 2041 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Experiment for Drug Resistance |
Disk diffusion assay | |||
| Mechanism Description | Using the Ery- strain AR1807 as a recipient for plasmid-directed integrative recombination, the chromosomal ermR gene (encoding 23S rRNA methyltransferase) was disrupted, ermR-disrupted strains AR1848 and AR1849 were highly sensitive to erythromycin and the other macrolide antibiotics. Phenotypic characterizations demonstrated that ermR is the sole determinant of macrolide antibiotic resistance in A. erythreum. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: rRNA adenine N-6-methyltransferase (ErmB) | [27] | |||
| Resistant Disease | Clostridium difficile infection [ICD-11: 1A04.0] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Mechanism Description | The cellular methylation in C. difficile has been proposed to induce resistance to macrolides (erythromycin, ERY), lincosamide (clindamycin) and streptogramin B antibiotic family. These drugs target at a bacterial 50S ribosomal subunit, causing the inhibition of peptide chain growth by blocking the movement of ribosome. ERY ribosomal methylase B (ErmB) is responsible for ribosomal methylation at the specific site of 23S rRNA, resulting in the prevention of antibiotic binding. | |||
|
|
||||
| Key Molecule: Major facilitator superfamily (MFS) | [27] | |||
| Resistant Disease | Clostridium difficile infection [ICD-11: 1A04.0] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Mechanism Description | In C. difficile, two secondary active transporters belonging to the MFS and MATE families have been reported to be associated with drug resistance. Heterologous expression of the clostridial Cme protein in the MFS subfamily promotes ERY resistance in Enterococcus faecalis. A sodium-dependent efflux pump of the MATE subfamily encoded by the cdeA gene of C. difficile attributes resistance to norfloxacin and ciprofloxacin when the gene was overexpressed in Escherichia coli. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Macrolide export ATP-binding/permease protein MacB (MACB) | [17] | |||
| Resistant Disease | Salmonella enterica infection [ICD-11: 1A09.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Salmonella enterica serovar Typhimurium ATCC 14028s | 588858 | ||
| Experiment for Molecule Alteration |
Quantitative real-time PCR | |||
| Experiment for Drug Resistance |
L agar plate method assay | |||
| Mechanism Description | Overexpression or overproduction of macAB confers drug resistance. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Superficial skin infection by Staphylococcus aureus infection [ICD-11: 1B21.3] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: 23S ribosomal RNA methyltransferase Erm (ERM39) | [14] | |||
| Resistant Disease | Mycobacterium fortuitum infection [ICD-11: 1B2Z.2] | |||
| Molecule Alteration | Missense mutation | Putative initiation codon GTG>CTG |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Mycobacterium peregrinum ATCC14467 | 43304 | ||
| Experiment for Molecule Alteration |
DNA sequencing assay | |||
| Experiment for Drug Resistance |
Mueller-Hinton (MH) broth assay | |||
| Mechanism Description | The erm genes are a diverse collection of methylases that add one or two methyl groups to the adenine at position 2058 (Escherichia coli numbering) of the 23S rRNA; this modification impairs the binding of macrolides to ribosomes, and thus reduces the inhibitory activity of these agents. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Macrolide-lincosamide-streptogramin B resistance protein (ERMA) | [20] | |||
| Resistant Disease | Streptococcus pyogenes infection [ICD-11: 1A00-1C4Z] | |||
| Molecule Alteration | Methylation | Macrolide-binding site on the ribosome |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli AG100A | 562 | ||
| Experiment for Molecule Alteration |
PCR amplification and sequence alignments assay | |||
| Experiment for Drug Resistance |
Agar dilution method assay | |||
| Mechanism Description | Macrolide resistance commonly occurs due to methylation of the macrolide-binding site on the ribosome by methyltransferases encoded by the erm group of genes, Induction of erm(A) occurs by translational attenuationInduction of erm(A) occurs by translational attenuation. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: 23S rRNA (cytidine-2'-O)-methyltransferase TlyA (TLYA) | [22] | |||
| Resistant Disease | Bordetella pertussis infection [ICD-11: 1C12.0] | |||
| Molecule Alteration | Missense mutation | p.A2047G |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Bordetella pertussis isolate | 1952 | ||
| Experiment for Molecule Alteration |
Whole genome sequencing assay | |||
| Experiment for Drug Resistance |
Disk diffusion assay | |||
| Mechanism Description | All of the strains of B. pertussis resistant to erythromycin in our center had the A2047G mutation of the 23S rRNA gene. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Oleandomycin glycosyltransferase oleD (OLED) | [6] | |||
| Resistant Disease | Streptomyces infection [ICD-11: 1C43.6] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli C41(DE3) | 469008 | ||
| Experiment for Molecule Alteration |
Linked enzyme activity assay | |||
| Experiment for Drug Resistance |
MIC assay | |||
| Mechanism Description | Glycosylation of macrolide antibiotics confers host cell immunity from endogenous and exogenous agents. The Streptomyces antibioticus glycosyltransferases, OleD, diverse macrolides including erythromycin. | |||
| Key Molecule: srmA open reading frame gimA (GIMA) | [23] | |||
| Resistant Disease | Streptomyces ambbyaciens infection [ICD-11: 1C43.0] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Escherichia coli | 668369 | ||
| Escherichia coli strain S17.1 | 1227813 | |||
| Micrococcus luteus strain Cgr | 1270 | |||
| Micrococcus luteus strain DSM1790 | 1270 | |||
| Streptomyces ambofaciens strain ATCC 23877 | 278992 | |||
| Streptomyces ambofaciens strain OS41.99 | 1954 | |||
| Streptomyces ambofaciens strain OS41.99NP | 1954 | |||
| Streptomyces ambofaciens strain OS81 | 1954 | |||
| Streptomyces lividans strain OS456 | 1916 | |||
| Experiment for Molecule Alteration |
DNA sequencing assay | |||
| Experiment for Drug Resistance |
Observation of growth inhibition zones assay | |||
| Mechanism Description | With UDP-[14C]glucose as the cofactor, crude S30 extracts from OS456(pOS41.90) were tested on various macrolides. Among those, chalcomycin was the most active substrate. Methymycin, tylosin, pikromycin, and rosaramicin were four of the best substrates. Oleandomycin, josamycin, and carbomycin were glycosylated to a lesser extent. Macrolides that were found to be as poor substrates of GimA as lankamycin were erythromycin and angolamycin. Spiramycin was also a very poor substrate. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: 23S ribosomal RNA methyltransferase Erm34 (ERM34) | [7] | |||
| Resistant Disease | Bacillus clausii infection [ICD-11: 1C4Y.1] | |||
| Molecule Alteration | Methylation | Ribosomal methylation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Bacillus clausii ATCC 21536 | 79880 | ||
| Experiment for Molecule Alteration |
Cloning experiments and gene seqencing assay | |||
| Experiment for Drug Resistance |
Agar dilution assay | |||
| Mechanism Description | This pattern of resistance generally due to the presence of an erm gene encoding a ribosomal methylase. | |||
| Key Molecule: rRNA adenine N-6-methyltransferase ermG (ERMG) | [41] | |||
| Resistant Disease | Bacillus sphaericus infection [ICD-11: 1C4Y.4] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Bacillus subtilis strain BD1107 | 1423 | ||
| Bacillus subtilis strain BD1117 | 1423 | |||
| Bacillus subtilis strain BD1146 | 1423 | |||
| Bacillus subtilis strain BD1156 | 1423 | |||
| Bacillus subtilis strain BD1158 | 1423 | |||
| Bacillus subtilis strain BD624 | 1423 | |||
| Bacillus subtilis strain BD629 | 1423 | |||
| Bacillus subtilis strain BD630 | 1423 | |||
| Bacillus subtilis strain CU403 | 1423 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Mechanism Description | One of the mechanisms of bacterial resistance to aminoglycosides is the production of aminoglycoside N-acetyl-transferase (AAC) enzymes which acetylate the amino groups present in the molecule of the aminoglycoside, preventing their interaction with the ribosome. ermG specifies a 29,000-dalton protein, the synthesis of which is induced by erythromycin. S1 nuclease mapping was used to identify the transcriptional start site. These experiments demonstrated the presence on the ermG mRNA of a 197 to 198-base leader. | |||
| Key Molecule: ErmR rRNA adenine N6-methyltransferase (ERMR) | [24] | |||
| Resistant Disease | Bacteroides fragilis infection [ICD-11: 1C4Y.6] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Bacteroides distasonis strains | 823 | ||
| Bacteroides distasonis strains V2002 | 823 | |||
| Bacteroides distasonis strains V2003 | 823 | |||
| Bacteroides distasonis strains V2004 | 823 | |||
| Bacteroides fragilis strain | 817 | |||
| Bacteroides fragilis strain V503 | 817 | |||
| Bacteroides ovatus strains | 28116 | |||
| Bacteroides ovatus strains V2008 | 28116 | |||
| Bacteroides thetaiotaomicron strain | 818 | |||
| Bacteroides thetaiotaomicron strain V2005 | 818 | |||
| Bacteroides thetaiotaomicron strain V2006 | 818 | |||
| Bacteroides thetaiotaomicron strain V2007 | 818 | |||
| Bacteroides uniformis strain | 820 | |||
| Bacteroides uniformis strain V1760 | 820 | |||
| Bacteroides uniformis strain V1761 | 820 | |||
| Bacteroides uniformis strain V1918 | 820 | |||
| Bacteroides uniformis strain V1921 | 820 | |||
| Bacteroides uniformis strain V2000 | 820 | |||
| Bacteroides uniformis strain V2001 | 820 | |||
| Bacteroides uniformis strain V528 | 820 | |||
| Bacteroides uniformis strain V844 | 820 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Mechanism Description | Clindamycin resistance in Bacteroides spp. is usually macrolide-lincosamide-streptogramin B (MLS) resistance conferred by erm genes which are similar to those seen in gram-positive, facultative anaerobes. Of 13 clinical isolates of the Bacteroides group, all were resistant to tetracycline (>10,ug/ml). Seven of the eight clindamycin-resistant clinical isolates constitutively expressed erythromycin resistance and had a high level of resistance to clindamycin (> 10ug/ml). V2002 was susceptible to erythromycin. | |||
| Key Molecule: ErmR rRNA adenine N6-methyltransferase (ERMR) | [24] | |||
| Resistant Disease | Bacteroides thetaiotaomicron infection [ICD-11: 1C4Y.10] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Bacteroides distasonis strains | 823 | ||
| Bacteroides distasonis strains V2002 | 823 | |||
| Bacteroides distasonis strains V2003 | 823 | |||
| Bacteroides distasonis strains V2004 | 823 | |||
| Bacteroides fragilis strain | 817 | |||
| Bacteroides fragilis strain V503 | 817 | |||
| Bacteroides ovatus strains | 28116 | |||
| Bacteroides ovatus strains V2008 | 28116 | |||
| Bacteroides thetaiotaomicron strain | 818 | |||
| Bacteroides thetaiotaomicron strain V2005 | 818 | |||
| Bacteroides thetaiotaomicron strain V2006 | 818 | |||
| Bacteroides thetaiotaomicron strain V2007 | 818 | |||
| Bacteroides uniformis strain | 820 | |||
| Bacteroides uniformis strain V1760 | 820 | |||
| Bacteroides uniformis strain V1761 | 820 | |||
| Bacteroides uniformis strain V1918 | 820 | |||
| Bacteroides uniformis strain V1921 | 820 | |||
| Bacteroides uniformis strain V2000 | 820 | |||
| Bacteroides uniformis strain V2001 | 820 | |||
| Bacteroides uniformis strain V528 | 820 | |||
| Bacteroides uniformis strain V844 | 820 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Mechanism Description | Clindamycin resistance in Bacteroides spp. is usually macrolide-lincosamide-streptogramin B (MLS) resistance conferred by erm genes which are similar to those seen in gram-positive, facultative anaerobes. Of 13 clinical isolates of the Bacteroides group, all were resistant to tetracycline (>10,ug/ml). Seven of the eight clindamycin-resistant clinical isolates constitutively expressed erythromycin resistance and had a high level of resistance to clindamycin (> 10ug/ml). V2002 was susceptible to erythromycin. | |||
| Key Molecule: ErmR rRNA adenine N6-methyltransferase (ERMR) | [24] | |||
| Resistant Disease | Bacteroides ovatus infection [ICD-11: 1C4Y.8] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Bacteroides distasonis strains | 823 | ||
| Bacteroides distasonis strains V2002 | 823 | |||
| Bacteroides distasonis strains V2003 | 823 | |||
| Bacteroides distasonis strains V2004 | 823 | |||
| Bacteroides fragilis strain | 817 | |||
| Bacteroides fragilis strain V503 | 817 | |||
| Bacteroides ovatus strains | 28116 | |||
| Bacteroides ovatus strains V2008 | 28116 | |||
| Bacteroides thetaiotaomicron strain | 818 | |||
| Bacteroides thetaiotaomicron strain V2005 | 818 | |||
| Bacteroides thetaiotaomicron strain V2006 | 818 | |||
| Bacteroides thetaiotaomicron strain V2007 | 818 | |||
| Bacteroides uniformis strain | 820 | |||
| Bacteroides uniformis strain V1760 | 820 | |||
| Bacteroides uniformis strain V1761 | 820 | |||
| Bacteroides uniformis strain V1918 | 820 | |||
| Bacteroides uniformis strain V1921 | 820 | |||
| Bacteroides uniformis strain V2000 | 820 | |||
| Bacteroides uniformis strain V2001 | 820 | |||
| Bacteroides uniformis strain V528 | 820 | |||
| Bacteroides uniformis strain V844 | 820 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Mechanism Description | Clindamycin resistance in Bacteroides spp. is usually macrolide-lincosamide-streptogramin B (MLS) resistance conferred by erm genes which are similar to those seen in gram-positive, facultative anaerobes. Of 13 clinical isolates of the Bacteroides group, all were resistant to tetracycline (>10,ug/ml). Seven of the eight clindamycin-resistant clinical isolates constitutively expressed erythromycin resistance and had a high level of resistance to clindamycin (> 10ug/ml). V2002 was susceptible to erythromycin. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: 23S rRNA (cytidine-2'-O)-methyltransferase TlyA (TLYA) | [26] | |||
| Resistant Disease | Mycoplasma pneumoniae infection [ICD-11: 1D01.3] | |||
| Molecule Alteration | Missense mutation | p.A2063G+p.A2064G+p.A2617G |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| In Vitro Model | Mycoplasma pneumoniae strain | 2014 | ||
| Experiment for Drug Resistance |
MIC assay | |||
| Mechanism Description | It has been confirmed that drug resistance to macrolide antibiotics of MP is mainly related to the mutation of Gene 23SrRNA in Area V, most commonly in the mutation of A2063G and followed by A2064G and A2617G. Rarely, mutation of ribosomal protein L4 or L22 may induce drug resistance to macrolide antibiotics. | |||
| Key Molecule: 23s rRNA | [12] | |||
| Resistant Disease | Acinetobacter meningitis [ICD-11: 1D01.1] | |||
| Molecule Alteration | Missense mutation | c.421C>A (rs2231142) |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | M. pneumoniae M129 | 2093 | ||
| Experiment for Molecule Alteration |
GeneSeq assay; PCR | |||
| Experiment for Drug Resistance |
Antimicrobial susceptibility assay | |||
| Mechanism Description | Since the secondary treatment choice for pediatric patients is very limited, we decided to look for potential new treatment strategies in macrolide drugs and investigate possible new mechanisms of resistance. We performed an in vitro selection of mutants resistant to five macrolides (erythromycin, roxithromycin, azithromycin, josamycin, and midecamycin) by inducing the parent M. pneumoniae strain M129 with increasing concentrations of the drugs. The evolving cultures in every passage were tested for their antimicrobial susceptibilities to eight drugs and mutations known to be associated with macrolide resistance by PCR and sequencing. The final selected mutants were also analyzed by whole-genome sequencing. Results showed that roxithromycin is the drug that most easily induces resistance (at 0.25 mg/L, with two passages, 23 days), while with midecamycin it is most difficult (at 5.12 mg/L, with seven passages, 87 days). Point mutations C2617A/T, A2063G, or A2064C in domain V of 23S rRNA were detected in mutants resistant to the 14- and 15-membered macrolides, while A2067G/C was selected for the 16-membered macrolides. Single amino acid changes (G72R, G72V) in ribosomal protein L4 emerged during the induction by midecamycin. Genome sequencing identified sequence variations in dnaK, rpoC, glpK, MPN449, and in one of the hsdS (MPN365) genes in the mutants. Mutants induced by the 14- or 15-membered macrolides were resistant to all macrolides, while those induced by the 16-membered macrolides (midecamycin and josamycin) remained susceptible to the 14- and 15-membered macrolides. In summary, these data demonstrated that midecamycin is less potent in inducing resistance than other macrolides, and the induced resistance is restrained to the 16-membered macrolides, suggesting a potential benefit of using midecamycin as a first treatment choice if the strain is susceptible. | |||
|
|
||||
| Key Molecule: MsrC (MSRC) | [11] | |||
| Resistant Disease | Enterococcus faecium meningitis [ICD-11: 1D01.2] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli | 668369 | ||
| Enterococcus faecium TX2465 | 1352 | |||
| Escherichia coli TX1330 | 668369 | |||
| Escherichia coli TX2046 | 668369 | |||
| Escherichia coli TX2597 | 668369 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Experiment for Drug Resistance |
Twofold dilutions assay | |||
| Mechanism Description | The complete sequence (1,479 nucleotides) of msrC, part of which was recently reported by others using a different strain, was determined. This gene was found in 233 of 233 isolates of Enterococcus faecium but in none of 265 other enterococci. Disruption of msrC was associated with a two- to eightfold decrease in MICs of erythromycin azithromycin, tylosin, and quinupristin, suggesting that it may explain in part the apparent greater intrinsic resistance to macrolides of isolates of E. faecium relative to many streptococci. This endogenous, species-specific gene of E. faecium is 53% identical to msr(A), suggesting that it may be a remote progenitor of the acquired macrolide resistance gene found in some isolates of staphylococci. | |||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: MsrC (MSRC) | [11] | |||
| Sensitive Disease | Enterococcus faecium meningitis [ICD-11: 1D01.2] | |||
| Molecule Alteration | Truncated mutantion | Disruption (nt 1251 to 1879) |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli | 668369 | ||
| Enterococcus faecium TX2465 | 1352 | |||
| Escherichia coli TX1330 | 668369 | |||
| Escherichia coli TX2046 | 668369 | |||
| Escherichia coli TX2597 | 668369 | |||
| Experiment for Molecule Alteration |
Southern blotting assay | |||
| Experiment for Drug Resistance |
Twofold dilutions assay | |||
| Mechanism Description | Disruption of msrC was associated with a two- to eightfold decrease in MICs of erythromycin azithromycin, tylosin, and quinupristin, suggesting that it may explain in part the apparent greater intrinsic resistance to macrolides of isolates of E. faecium relative to many streptococci. | |||
ICD-11: Circulatory system diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
ICD-12: Respiratory system diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Erythromycin esterase (EREA2) | [42] | |||
| Resistant Disease | Community-acquired pneumonia [ICD-11: CA40.2] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli BL21(DE3) | 469008 | ||
| Escherichia coli TOP10 | 83333 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Disk diffusion test assay; E-strip test assay | |||
| Mechanism Description | One mechanism of macrolide resistance is via drug inactivation: enzymatic hydrolysis of the macrolactone ring catalyzed by erythromycin esterases, EreA and EreB. | |||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
| Key Molecule: Multidrug efflux SMR transporter (ABES) | [43] | |||
| Resistant Disease | Acinetobacter baumannii infection [ICD-11: CA40.4] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Experiment for Molecule Alteration |
Fluorometric efflux assay | |||
| Experiment for Drug Resistance |
Broth dilution assay | |||
| Mechanism Description | The abeS gene product conferred resistance to various antimicrobial compounds through an efflux mechanism. | |||
| Key Molecule: MATE family efflux transporter (ABEM) | [16] | |||
| Resistant Disease | Acinetobacter baumannii infection [ICD-11: CA40.4] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Experiment for Drug Resistance |
MIC assay | |||
| Mechanism Description | AbeM was found to be an H+-coupled multidrug efflux pump and a unique member of the MATE family which lead to drug resistance. | |||
ICD-21: Symptoms/clinical signs/unclassified clinical findings
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
ICD-22: Injury/poisoning/certain external causes consequences
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Erythromycin resistance protein (ERM38) | [21] | |||
| Resistant Disease | Mycobacterium smegmatis infection [ICD-11: 1B2Z.3] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Mycobacterium smegmatis mc2155 | 246196 | ||
| Mycobacterium smegmatis mc2155/pMIP12 | 246196 | |||
| Mycobacterium smegmatis mc2155/pOMV20 | 246196 | |||
| Mycobacterium smegmatis mc2155/pOMV30 | 246196 | |||
| Experiment for Molecule Alteration |
MALDI mass spectrometry assay | |||
| Experiment for Drug Resistance |
MIC assay | |||
| Mechanism Description | Erm (38) is a specific dimethyltransferase. The strain obtained drug resistance by adding two methyl groups to A2058 in Mycobacterium 23SrRNA. | |||
| Key Molecule: Erythromycin resistance protein (ERM38) | [21] | |||
| Resistant Disease | Mycobacterium smegmatis infection [ICD-11: 1B2Z.3] | |||
| Molecule Alteration | Expression | Inherence |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Mycobacterium smegmatis mc2155 | 246196 | ||
| Mycobacterium smegmatis mc2155/pMIP12 | 246196 | |||
| Mycobacterium smegmatis mc2155/pOMV20 | 246196 | |||
| Mycobacterium smegmatis mc2155/pOMV30 | 246196 | |||
| Experiment for Molecule Alteration |
MALDI mass spectrometry assay | |||
| Experiment for Drug Resistance |
MIC assay | |||
| Mechanism Description | Erm (38) is a specific dimethyltransferase. The strain obtained drug resistance by adding two methyl groups to A2058 in Mycobacterium 23SrRNA. | |||
|
|
||||
| Key Molecule: Lincomycin resistance efflux pump (LMRS) | [8] | |||
| Resistant Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vitro Model | Escherichia coli kAM32 | 562 | ||
| Staphylococcus aureus OM505 | 1280 | |||
| Experiment for Molecule Alteration |
Whole genome sequence assay; Allelic frequency measurement assay | |||
| Experiment for Drug Resistance |
Broth microdilution method assay | |||
| Mechanism Description | LmrS is a multidrug efflux pump of the major facilitator superfamily from staphylococcus aureus. | |||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
