Drug Information
Drug (ID: DG00112) and It's Reported Resistant Information
| Name |
Cytarabine
|
||||
|---|---|---|---|---|---|
| Synonyms |
Alexan; AraC; Arabinocytidine; Arabinofuranosylcytosine; Arabinosylcytosine; Arabitin; Aracytidine; Aracytin; Aracytine; Arafcyt; Citarabina; Cytarabin; Cytarabina; Cytarabinoside; Cytarabinum; Cytarbel; Cytonal; Cytosar; Cytosinearabinoside; DepoCyte; Depocyt; Erpalfa; Iretin; Spongocytidine; Tarabine; Udicil; Arabinosyl Cytosine; Cytarabine liposome injection; Cytosine arabinofuranoside; Cytosine arabinose; Cytosine arabinoside; AR3; BTB15125; CHX 3311; U 19920A; Ara-C; Ara-Cytidine; Beta-Ara C; Beta-Arabinosylcytosine; Beta-cytosine arabinoside; Citarabina [INN-Spanish]; Cytarabinum [INN-Latin]; Cytosar-U; Cytosine arabinoside (VAN); Depocyt (TN); Depocyt (liposomal); Intrathecal (injected into the spinal fluid) DepoCyt; U-19920; Beta-D-Arabinosylcytosine; Cytosar-U (TN); Cytosine beta-D-arabinofuranoside; Cytosine beta-D-arabinofuranoside hydrochloride; Cytosine beta-D-arabinoside; Cytosine-beta-arabinoside; Intrathecal cytarabine (also known as ara-C); U-19,920; CYTARABINE (SEE ALSO CYTARABINE HYDROCHLORIDE 69-74-9); Cytarabine (JP15/USP/INN); Cytarabine [USAN:INN:BAN:JAN]; Cytosine 1-beta-D-arabinofuranoside; Cytosine, beta-D-arabinoside; Cytosine-beta-D-arabinofuranoside; Cytosine-1-beta-D-arabinofuranoside; Ara-C, Cytosine Arabinoside, Cytosar-U, Cytarabine; (beta-D-Arabinofuranosyl)cytosine; 1-.beta.-D-arabinofuranosyl-cytosine; 1-Arabinofuranosylcytosine; 1-beta-D-Arabinofaranosylcytosine; 1-beta-D-Arabinofuranosyl-4-amino-2(1H)pyrimidinone; 1-beta-D-Arabinofuranosylcytosine; 1-beta-D-Arabinofuranosylcytosine, Cytosine Arabinoside; 1-beta-D-Arabinosylcytosine; 1beta-Arabinofuranasylcytosine; 1beta-D-Arabinofuranosylcytosine; 1beta-D-Arabinosylcytosine; 2(1H)-Pyrimidinone, 4-amino-1-D-arabinofuranosyl-[CAS]; 4-Amino-1-arabinofuranosyl-2-oxo-1,2-dihydropyrimidin; 4-Amino-1-arabinofuranosyl-2-oxo-1,2-dihydropyrimidin [Czech]; 4-Amino-1-arabinofuranosyl-2-oxo-1,2-dihydropyrimidine; 4-Amino-1-b-D-arabinofuranosyl-2-(1H)-pyrimidinone; 4-Amino-1-beta-D-arabinofuranosyl-2(1H)-pyrimidinon; 4-Amino-1-beta-D-arabinofuranosyl-2(1H)-pyrimidinon [Czech]; 4-Amino-1-beta-D-arabinofuranosyl-2(1H)-pyrimidinone; 4-amino-1-[(2R,3S,4S,5R)-3,4-dihydroxy-5-(hydroxymethyl)oxolan-2-yl]pyrimidin-2-one; 4-amino-1-beta-D-arabinofuranosylpyrimidin-2(1H)-one
Click to Show/Hide
|
||||
| Indication |
In total 1 Indication(s)
|
||||
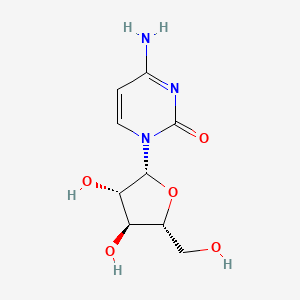
| Structure |
|
||||
| Drug Resistance Disease(s) |
Disease(s) with Clinically Reported Resistance for This Drug
(4 diseases)
[2]
[1]
[2]
[3]
Disease(s) with Resistance Information Discovered by Cell Line Test for This Drug
(2 diseases)
[4]
[5]
|
||||
| Target | Herpes simplex virus DNA polymerase UL30 (HSV UL30) | DPOL_HHV11 | [1] | ||
| Click to Show/Hide the Molecular Information and External Link(s) of This Drug | |||||
| Formula |
C9H13N3O5
|
||||
| IsoSMILES |
C1=CN(C(=O)N=C1N)[C@H]2[C@H]([C@@H]([C@H](O2)CO)O)O
|
||||
| InChI |
1S/C9H13N3O5/c10-5-1-2-12(9(16)11-5)8-7(15)6(14)4(3-13)17-8/h1-2,4,6-8,13-15H,3H2,(H2,10,11,16)/t4-,6-,7+,8-/m1/s1
|
||||
| InChIKey |
UHDGCWIWMRVCDJ-CCXZUQQUSA-N
|
||||
| PubChem CID | |||||
| ChEBI ID | |||||
| TTD Drug ID | |||||
| VARIDT ID | |||||
| INTEDE ID | |||||
| DrugBank ID | |||||
Type(s) of Resistant Mechanism of This Drug
Drug Resistance Data Categorized by Their Corresponding Diseases
ICD-02: Benign/in-situ/malignant neoplasm
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vitro Model | KG-1 A cells | Blood | Homo sapiens (Human) | CVCL_0374 |
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | In this study, we find that TGFB1 levels are elevated in relapsed or refractory AML patients and in drug-resistant cell lines, and can induce chemoresistance by stimulating the activation of the TGFB signaling pathway via an autocrine/paracrine manner. This process may be achieved through metabolic reprogramming induced by TGFB1-triggered SOX9 expression. | |||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vitro Model | K562/ADR cells | Blood | Homo sapiens (Human) | CVCL_0004 |
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | In this study, we find that TGFB1 levels are elevated in relapsed or refractory AML patients and in drug-resistant cell lines, and can induce chemoresistance by stimulating the activation of the TGFB signaling pathway via an autocrine/paracrine manner. This process may be achieved through metabolic reprogramming induced by TGFB1-triggered SOX13 expression. | |||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vitro Model | HL60/ADR cells | Blood | Homo sapiens (Human) | CVCL_0002 |
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | In this study, we find that TGFB1 levels are elevated in relapsed or refractory AML patients and in drug-resistant cell lines, and can induce chemoresistance by stimulating the activation of the TGFB signaling pathway via an autocrine/paracrine manner. This process may be achieved through metabolic reprogramming induced by TGFB1-triggered SOX12 expression. | |||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vitro Model | K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 |
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | In this study, we find that TGFB1 levels are elevated in relapsed or refractory AML patients and in drug-resistant cell lines, and can induce chemoresistance by stimulating the activation of the TGFB signaling pathway via an autocrine/paracrine manner. This process may be achieved through metabolic reprogramming induced by TGFB1-triggered SOX11 expression. | |||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vitro Model | HL-60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | In this study, we find that TGFB1 levels are elevated in relapsed or refractory AML patients and in drug-resistant cell lines, and can induce chemoresistance by stimulating the activation of the TGFB signaling pathway via an autocrine/paracrine manner. This process may be achieved through metabolic reprogramming induced by TGFB1-triggered SOX10 expression. | |||
| Key Molecule: Transforming growth factor beta 1 (TGFB1) | [5] | |||
| Metabolic Type | Lipid metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myeloid leukemia | |||
| The Studied Tissue | Blood | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.40E-07 Fold-change: 6.20E-01 Z-score: 6.08E+00 |
|||
| Experimental Note | Identified from the Human Clinical Data | |||
| Cell Pathway Regulation | TGF-beta signaling pathway | Activation | hsa04350 | |
| In Vivo Model | HCC patients | Homo Sapiens | ||
| Experiment for Molecule Alteration |
qRT-PCR; Western blot analysis | |||
| Key Molecule: Cytochrome P450 family 1 subfamily A member 1 (CYP1A1) | [8] | |||
| Metabolic Type | Mitochondrial metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cushing syndrome | Activation | hsa04934 | |
| In Vitro Model | SHI-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_2191 |
| Skm1 cells | Blood | Homo sapiens (Human) | CVCL_0098 | |
| U937 cells | Blood | Homo sapiens (Human) | CVCL_0007 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
Cell viability assay | |||
| Mechanism Description | The data analysis reveals that the AHR signaling pathway is activated in AML patients. Furthermore, there is a correlation between the expressions of AHR and mitochondrial oxidative phosphorylation genes.In vitroexperiments show that enhancing AHR expression in AML cells increases mitochondrial oxidative phosphorylation and induces resistance to cytarabine. Conversely, reducing AHR expression in AML cells decreases cytarabine resistance. | |||
| Key Molecule: Cytochrome P450 family 1 subfamily B member 1 (CYP1B1) | [8] | |||
| Metabolic Type | Mitochondrial metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cushing syndrome | Activation | hsa04934 | |
| In Vitro Model | SHI-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_2191 |
| Skm1 cells | Blood | Homo sapiens (Human) | CVCL_0098 | |
| U937 cells | Blood | Homo sapiens (Human) | CVCL_0007 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
Cell viability assay | |||
| Mechanism Description | The data analysis reveals that the AHR signaling pathway is activated in AML patients. Furthermore, there is a correlation between the expressions of AHR and mitochondrial oxidative phosphorylation genes.In vitroexperiments show that enhancing AHR expression in AML cells increases mitochondrial oxidative phosphorylation and induces resistance to cytarabine. Conversely, reducing AHR expression in AML cells decreases cytarabine resistance. | |||
| Key Molecule: Isocitrate dehydrogenase [NADP] mitochondrial (IDH2) | [9] | |||
| Metabolic Type | Glucose metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Mutation | . |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Longevity regulating pathway - multiple species | Activation | hsa04213 | |
| In Vitro Model | AML cells | N.A. | Homo sapiens (Human) | N.A. |
| HL-60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 | |
| IDH2 mutant AML cells | Blood | Homo sapiens (Human) | CVCL_S481 | |
| KG-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_0374 | |
| Experiment for Drug Resistance |
IC50 assay | |||
| Mechanism Description | The increase in glycolysis levels following IDH2 mutation may contribute to the reduced efficacy of Enasidenib in inhibiting the proliferation of IDH-mutant AML cells. | |||
| Key Molecule: Isocitrate dehydrogenase [NADP] mitochondrial (IDH2) | [9] | |||
| Metabolic Type | Glucose metabolism | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Mutation | . |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Longevity regulating pathway - multiple species | Activation | hsa04213 | |
| In Vivo Model | AML cell-transplanted tumor nude mice with IDH2 mutations | Mice | ||
| Experiment for Drug Resistance |
Tumor volume assay | |||
| Mechanism Description | The increase in glycolysis levels following IDH2 mutation may contribute to the reduced efficacy of Enasidenib in inhibiting the proliferation of IDH-mutant AML cells. | |||
| Key Molecule: Dihydrofolate reductase (DHFR) | [10] | |||
| Metabolic Type | Nucleic acid metabolism | |||
| Resistant Disease | Acute promyelocytic leukemia [ICD-11: 2A60.2] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | THP1 cells | Pleural effusion | Homo sapiens (Human) | CVCL_0006 |
| Experiment for Molecule Alteration |
qRT-PCR | |||
| Experiment for Drug Resistance |
Cell viability assay | |||
| Mechanism Description | Here, we use genome-scale metabolic modelling to reconstruct a GSMM of the THP1 AML cell line and two derivative cell lines, one with acquired resistance to AraC and the second with acquired resistance to DOX. We also explore how, adding to the transcriptomic layer, the metabolomic layer enhances the selectivity of the resulting condition specific reconstructions. The resulting models enabled us to identify and experimentally validate that drug-resistant THP1 cells are sensitive to the FDA-approved antifolate methotrexate. | |||
| Key Molecule: Squalene synthase (FDFT1) | [10] | |||
| Metabolic Type | Nucleic acid metabolism | |||
| Resistant Disease | Acute promyelocytic leukemia [ICD-11: 2A60.2] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | THP1 cells | Pleural effusion | Homo sapiens (Human) | CVCL_0006 |
| Experiment for Molecule Alteration |
qRT-PCR | |||
| Experiment for Drug Resistance |
Cell viability assay | |||
| Mechanism Description | Here, we use genome-scale metabolic modelling to reconstruct a GSMM of the THP1 AML cell line and two derivative cell lines, one with acquired resistance to AraC and the second with acquired resistance to DOX. We also explore how, adding to the transcriptomic layer, the metabolomic layer enhances the selectivity of the resulting condition specific reconstructions. The resulting models enabled us to identify and experimentally validate that drug-resistant THP1 cells are sensitive to the FDA-approved antifolate methotrexate. | |||
|
|
||||
| Key Molecule: hsa-mir-335 | [1] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Cell Pathway Regulation | Cell apoptosis | Inhibition | hsa04210 | |
| Cell invasion | Activation | hsa05200 | ||
| Cell migration | Activation | hsa04670 | ||
| Cell proliferation | Activation | hsa05200 | ||
| Nodal/TFG-alpha signaling pathway | Regulation | N.A. | ||
| Wnt/alpha -catenin signaling pathway | Regulation | N.A. | ||
| Experiment for Molecule Alteration |
RT-qPCR | |||
| Experiment for Drug Resistance |
Relapse-free survival and overall survival assay | |||
| Mechanism Description | The expression levels of miR-335 in bone marrow and serum samples from adult patients with AML (except M3) were significantly associated with the Ara-C-based chemotherapy response and clinical outcome after treatment. | |||
|
|
||||
| Key Molecule: Isocitrate dehydrogenase NADP 2 (IDH2) | [11] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | PI3K/Akt/mTOR signaling pathway | Regulation | N.A. | |
| In Vitro Model | HL-60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| KG-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_0374 | |
| In Vivo Model | SPF-grade (BALB/C) nude mice model | Mus musculus | ||
| Experiment for Molecule Alteration |
RT-qPCR; Glycolysis metabolic enzyme assay; Flow cytometry; Western blot assay; Transcriptome sequencingc assay | |||
| Experiment for Drug Resistance |
Cell proliferation assay; Drug sensitivity testing | |||
| Mechanism Description | OE-IDH2 in AML cells, enhances resistance to the Ara-C, promotes cell proliferation and glycolysis, and inhibits apoptosis. KD-IDH2 exhibits opposite effects. Both IDH2 mutations and OE-IDH2 produce similar effects on these cellular processes. The increase in glycolysis levels following IDH2 mutation may contribute to the reduced efficacy of Enasidenib in inhibiting the proliferation of IDH-mutant AML cells. Transcriptome sequencing results indicate an enrichment of the PI3K/Akt signaling pathway in IDH2-mutant AML cells. BEZ235 significantly inhibits the expression of phosphorylated PI3K (p-PI3K), phosphorylated Akt (p-Akt), mTOR, glycolytic metabolism, and Ara-C resistance both in vitro and in vivo. Overexpression and mutation of IDH2 coordinate with the Warburg effect through the PI3K/Akt/mTOR pathway to promote Ara-C resistance in AML. | |||
| Key Molecule: Isocitrate dehydrogenase [NADP] mitochondrial (IDH2) | [11] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Mutation | . |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | PI3K-Akt signaling pathway | Activation | hsa04151 | |
| In Vitro Model | HL-60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| KG-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_0374 | |
| Experiment for Drug Resistance |
Flow cytometry assay | |||
| Mechanism Description | The IDH2 mutations are involved in Ara-C resistance by affecting the process of glycolysis in AML, and the PI3K-Akt signaling pathway plays an important role in this process. These pathways are expected to be important targets for targeted therapeutic intervention in the AML setting. | |||
| Key Molecule: Acetyl-CoA acetyltransferase 2 (ACAT2) | [12] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | DNA Damage Response Mechanism | Regulation | N.A. | |
| In Vitro Model | MV-4-11 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0064 |
| MOLM-13 cells | Peripheral blood | Homo sapiens (Human) | CVCL_2119 | |
| Kasumi-1 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0589 | |
| TF-1 cells | Blood | Homo sapiens (Human) | CVCL_0559 | |
| Experiment for Molecule Alteration |
RT-qPCR; Western blot assay | |||
| Experiment for Drug Resistance |
MTT assay; Trypan blue assay; Clonogenicity assay; IC50 assay; Flow cytometry assay | |||
| Mechanism Description | DNA Damage Response Mechanism (DDR) comprises numerous molecules and pathways intended to arrest the cell cycle until DNA damage is repaired or else drive the cell to apoptosis.DDR regulators demonstrate increased expression in patients with high cytogenetic risk possibly reflecting increased genotoxic stress. Especially, PPP1R15A is mainly involved in the recovery of the cells from stress and it was the only DDR gene upregulated in AML patients. | |||
| Key Molecule: Acetyl-CoA acetyltransferase 2 (ACAT2) | [12] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | DNA Damage Response Mechanism | Regulation | N.A. | |
| In Vitro Model | MV-4-11 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0064 |
| MOLM-13 cells | Peripheral blood | Homo sapiens (Human) | CVCL_2119 | |
| Kasumi-1 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0589 | |
| TF-1 cells | Blood | Homo sapiens (Human) | CVCL_0559 | |
| Experiment for Molecule Alteration |
RT-qPCR; Western blot assay | |||
| Experiment for Drug Resistance |
MTT assay; Trypan blue assay; Clonogenicity assay; IC50 assay; Flow cytometry assay | |||
| Mechanism Description | DNA Damage Response Mechanism (DDR) comprises numerous molecules and pathways intended to arrest the cell cycle until DNA damage is repaired or else drive the cell to apoptosis.DDR regulators demonstrate increased expression in patients with high cytogenetic risk possibly reflecting increased genotoxic stress.Using PCR arrays we observed an upregulation of of several DDR genes (CDKN1A, GADD45A, GADD45G, EXO1, and PPP1R15A) in KASUMI-1 and MV4-11 cell lines that survived following treatment with Idarubicin and Cytarabine. | |||
| Key Molecule: Growth arrest and DNA damage-inducible protein GADD45 gamma (GADD45G) | [12] | |||
| Resistant Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | DNA Damage Response Mechanism | Regulation | N.A. | |
| In Vitro Model | MV-4-11 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0064 |
| MOLM-13 cells | Peripheral blood | Homo sapiens (Human) | CVCL_2119 | |
| Kasumi-1 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0589 | |
| TF-1 cells | Blood | Homo sapiens (Human) | CVCL_0559 | |
| Experiment for Molecule Alteration |
RT-qPCR; Western blot assay | |||
| Experiment for Drug Resistance |
MTT assay; Trypan blue assay; Clonogenicity assay; IC50 assay; Flow cytometry assay | |||
| Mechanism Description | DNA Damage Response Mechanism (DDR) comprises numerous molecules and pathways intended to arrest the cell cycle until DNA damage is repaired or else drive the cell to apoptosis.DDR regulators demonstrate increased expression in patients with high cytogenetic risk possibly reflecting increased genotoxic stress.Using PCR arrays we observed an upregulation of of several DDR genes (CDKN1A, GADD45A, GADD45G, EXO1, and PPP1R15A) in KASUMI-1 and MV4-11 cell lines that survived following treatment with Idarubicin and Cytarabine. | |||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Programmed cell death protein 4 (PDCD4) | [6] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myelocytic leukemia | |||
| The Studied Tissue | Bone marrow | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 4.63E-03 Fold-change: 7.01E-02 Z-score: 2.85E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell apoptosis | Activation | hsa04210 | |
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | AMO-miR-21 significantly sensitizes HL60 cells to Ara-C byinducing apoptosis and these effects of AMO-miR-21 may be partially due to its up-regulation ofPDCD4. | |||
| Key Molecule: High mobility group protein B1 (HMGB1) | [7] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Differential expression of the molecule in resistant disease | ||||
| Classification of Disease | Acute myeloid leukemia [ICD-11: 2A60] | |||
| The Specified Disease | Acute myelocytic leukemia | |||
| The Studied Tissue | Bone marrow | |||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 3.67E-02 Fold-change: -9.69E-03 Z-score: -2.10E+00 |
|||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell apoptosis | Activation | hsa04210 | |
| Cell migration | Inhibition | hsa04670 | ||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | The ectopic expression of miR-181b in k562/A02 and HL-60/ADM cells robustly suppressed endogenous HMGB1 and Mcl-1 expression both at mRNA and protein levels. Conversely, knockdown of miR-181b by miR-181b inhibitor markedly increased the expression of both HMGB1 and Mcl-1. Restoration of miR-181b increased the drug sensitivity of AML MDR cells by targeting HMGB1 and Mcl-1. | |||
| Key Molecule: Klotho (KL) | [13] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Cell Pathway Regulation | AKTsignaling pathway | Inhibition | hsa04151 | |
| Cell apoptosis | Activation | hsa04210 | ||
| Cell proliferation | Inhibition | hsa05200 | ||
| In Vitro Model | KG-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_0374 |
| K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |
| HK-2 cells | Kidney | Homo sapiens (Human) | CVCL_0302 | |
| Experiment for Molecule Alteration |
RT-PCR; Western blot analysis | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | Transfection of the mimic miR-126-5p into the AML cell line, kG-1, resulted in a decrease in the sensitivity to cytarabin and the expression level of klotho mRNA as well as the elevation in the phosphorylation of Akt. The results of the present study demonstrated that higher expression levels of miR-126-5p/3p in patients with AML resulted in a poorer prognosis. Furthermore, miR-126-5p elevated the phosphorylation of Akt. | |||
| Key Molecule: Induced myeloid leukemia cell differentiation protein Mcl-1 (MCL1) | [7] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell apoptosis | Activation | hsa04210 | |
| Cell migration | Inhibition | hsa04670 | ||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | The ectopic expression of miR-181b in k562/A02 and HL-60/ADM cells robustly suppressed endogenous HMGB1 and Mcl-1 expression both at mRNA and protein levels. Conversely, knockdown of miR-181b by miR-181b inhibitor markedly increased the expression of both HMGB1 and Mcl-1. Restoration of miR-181b increased the drug sensitivity of AML MDR cells by targeting HMGB1 and Mcl-1. | |||
|
|
||||
| Key Molecule: hsa-miR-126-5p | [13] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Cell Pathway Regulation | AKTsignaling pathway | Inhibition | hsa04151 | |
| Cell apoptosis | Activation | hsa04210 | ||
| Cell proliferation | Inhibition | hsa05200 | ||
| In Vitro Model | KG-1 cells | Bone marrow | Homo sapiens (Human) | CVCL_0374 |
| K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |
| HK-2 cells | Kidney | Homo sapiens (Human) | CVCL_0302 | |
| Experiment for Molecule Alteration |
RT-PCR | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | Transfection of the mimic miR-126-5p into the AML cell line, kG-1, resulted in a decrease in the sensitivity to cytarabin and the expression level of klotho mRNA as well as the elevation in the phosphorylation of Akt. The results of the present study demonstrated that higher expression levels of miR-126-5p/3p in patients with AML resulted in a poorer prognosis. Furthermore, miR-126-5p elevated the phosphorylation of Akt. | |||
| Key Molecule: hsa-mir-181 | [7] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell apoptosis | Activation | hsa04210 | |
| Cell migration | Inhibition | hsa04670 | ||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |
| In Vivo Model | Nude mouse xenograft model | Mus musculus | ||
| Experiment for Molecule Alteration |
qRT-PCR | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | The ectopic expression of miR-181b in k562/A02 and HL-60/ADM cells robustly suppressed endogenous HMGB1 and Mcl-1 expression both at mRNA and protein levels. Conversely, knockdown of miR-181b by miR-181b inhibitor markedly increased the expression of both HMGB1 and Mcl-1. Restoration of miR-181b increased the drug sensitivity of AML MDR cells by targeting HMGB1 and Mcl-1. | |||
| Key Molecule: hsa-let-7a | [14] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell growth | Activation | hsa05200 | |
| Cell invasion | Activation | hsa05200 | ||
| Epithelial mesenchymal transition signaling pathway | Activation | hsa01521 | ||
| In Vitro Model | Molm13 cells | Blood | Homo sapiens (Human) | CVCL_2119 |
| OCI-AML3 cells | Blood | Homo sapiens (Human) | CVCL_1844 | |
| In Vivo Model | AML nude mouse xenograft model | Mus musculus | ||
| Experiment for Molecule Alteration |
RT-PCR | |||
| Experiment for Drug Resistance |
Flow cytometry assay | |||
| Mechanism Description | Xenografts of primary human AML cells engineered to overexpress let-7a exhibited enhanced sensitivity to cytarabine. | |||
| Key Molecule: Bcl-2-like protein 11 (BCL2L11) | [15] | |||
| Sensitive Disease | Myeloid leukemia [ICD-11: 2A60.4] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| U937 cells | Blood | Homo sapiens (Human) | CVCL_0007 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
Flow cytometry assay | |||
| Mechanism Description | One of the predicted targets of miR-32 lies in the 3' untranslated region (UTR) of BCL2L11 gene, which encodes the pro-apoptotic protein Bim, miR-32 blockade is sufficient to elevate Bim expression and sensitize AML cells to chemotherapy-induced apoptosis. | |||
| Key Molecule: hsa-mir-32 | [15] | |||
| Sensitive Disease | Myeloid leukemia [ICD-11: 2A60.4] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| U937 cells | Blood | Homo sapiens (Human) | CVCL_0007 | |
| Experiment for Molecule Alteration |
qRT-PCR | |||
| Experiment for Drug Resistance |
Flow cytometry assay | |||
| Mechanism Description | One of the predicted targets of miR-32 lies in the 3' untranslated region (UTR) of BCL2L11 gene, which encodes the pro-apoptotic protein Bim, miR-32 blockade is sufficient to elevate Bim expression and sensitize AML cells to chemotherapy-induced apoptosis. | |||
| Key Molecule: hsa-mir-21 | [6] | |||
| Sensitive Disease | Acute myeloid leukemia [ICD-11: 2A60.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | Cell apoptosis | Activation | hsa04210 | |
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| Experiment for Molecule Alteration |
RT-PCR | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | AMO-miR-21 significantly sensitizes HL60 cells to Ara-C byinducing apoptosis and these effects of AMO-miR-21 may be partially due to its up-regulation ofPDCD4. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Cytidine deaminase (CDA) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Also opposing the activation pathway are the two deaminase CDA and deoxycytidine monophosphate deaminase (dCMPD). Cytidine deaminase is a multi-subunit enzyme involved in the maintenance of the pyrimidine nucleotide pool within the cell and physiologically catalyzes the hydrolytic deamination of cytidine to uridine and deoxycytidine to deoxyuridine. In cytarabine biotransformation, CDA removes the amine group from its cytosine and converts the drug into the inactive uracil arabinoside derivative. | |||
| Key Molecule: Cardiolipin synthase (CLS) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | CMPD deaminates cytarabine-monophosphate to arabinosyl-uracil-monophosphate. A crucial role for this latter enzyme has been suggested in the metabolism of cytarabine-monophosphate in T-lymphoblastic leukemia. | |||
| Key Molecule: Deoxycytidine kinase (DCK) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Deoxycitidine kinase plays a pivotal role since phosphorylation of cytarabine preserves intracellular retention of the drug and prevents from inactivation to its uridine derivative, uracil arabinoside, by cytidine deaminase. The intracellular accumulation of cytarabine triphosphate, the active cytotoxic metabolite, is proportional to the cellular DCk level which has led to the conclusion that DCk enzyme retains a rate-limiting role for the activation of cytarabine. | |||
| Key Molecule: UMP-CMP kinase (CMPK1) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Activation of cytarabine occurs by means of the step wise de novo synthesis of 5'-mono-, di-, and triphosphate derivatives throughout the sequential action of deoxycytidine kinase (DCk), deoxycytidine monophosphate kinase (dCMk), and nucleoside diphosphate kinase (NDk) encoded by the NME1 gene. Phosphorylated cytarabine metabolites interfere with the cellular pool of natural nucleosides, are incorporated into DNA and inhibit DNA synthesis in a competitive fashion. In vitro studies have revealed that the intracellular concentrations of cytarabine-triphosphate are higher in cytarabine sensitive cells than in resistant cells. | |||
| Key Molecule: Nucleoside diphosphate kinase A (NME1) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Activation of cytarabine occurs by means of the step wise de novo synthesis of 5'-mono-, di-, and triphosphate derivatives throughout the sequential action of deoxycytidine kinase (DCk), deoxycytidine monophosphate kinase (dCMk), and nucleoside diphosphate kinase (NDk) encoded by the NME1 gene. Phosphorylated cytarabine metabolites interfere with the cellular pool of natural nucleosides, are incorporated into DNA and inhibit DNA synthesis in a competitive fashion. In vitro studies have revealed that the intracellular concentrations of cytarabine-triphosphate are higher in cytarabine sensitive cells than in resistant cells. | |||
| Key Molecule: Cytosolic purine 5'-nucleotidase (NT5C2) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Since monophosphorilated intermediate of cytarabine activation is reduced by cytosolic 5'-nucleotidases NT5C2 and NT5C3, the activity level of this enzyme may represent one of the factors affecting the clinical outcome of cytarabine therapy. Increased expression of NT5C2 has been correlated with resistance to cytarabine chemotherapy and to a lower survival rate in a hundred patients undergoing cytarabine chemotherapy. An increase in the NT5C2 has emerged as a mechanism of resistance to cytarabine. Patients with AML and low expression level of NT5C2 have a better overall survival after treatment with cytarabine than patients with high expression. NT5C2 is implicated in pharmacokinetic of cytarabine has been associated with poor clinical outcome. | |||
|
|
||||
| Key Molecule: ATP-binding cassette sub-family C10 (ABCC10) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Uptake and accumulation of cytarabine is also regulated by transmembrane transporter proteins of the ABC family, also called human multidrug resistance-associated protein (MRP) family, namely ABCC10 (MRP7) and ABCC11 (MRP8) specifically committed to efflux of deoxynucleotides inactive metabolites and to temper intracellular pools of phosphorylated deoxynucleotides. The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Key Molecule: ATP-binding cassette sub-family C11(ABCC11) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Uptake and accumulation of cytarabine is also regulated by transmembrane transporter proteins of the ABC family, also called human multidrug resistance-associated protein (MRP) family, namely ABCC10 (MRP7) and ABCC11 (MRP8) specifically committed to efflux of deoxynucleotides inactive metabolites and to temper intracellular pools of phosphorylated deoxynucleotides. The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Key Molecule: Solute carrier family 29 member 1 (SLC29A1) | [2] | |||
| Resistant Disease | Lymphoma [ICD-11: 2A90- 2A85] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Cytarabine gains entry into cells primarily as a false substrate through specialized nucleoside transporter proteins of SLC family, the human equilibrative nucleoside transportershENT1 and hENT2 (encoded by the gene SLC29A1 and SCL29A2, respectively) and the human concentrative nucleoside transporters hCNT3 (encoded by the gene SLC28A3). The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Cytidine deaminase (CDA) | [4] | |||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Jurkat cells | Pleural effusion | Homo sapiens (Human) | CVCL_0065 |
| Nalm-6 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0092 | |
| Experiment for Molecule Alteration |
Real-time quantitative PCR | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | Low-concentration cytarabine (Ara-C) continuously induced and cultured Jurkat and Nalm-6 cells to construct cytarabine-resistant cell lines Jurkat/Ara-C and Nalm-6/Ara-C. The results of real-time quantitative PCR showed that the expression of deoxycytidine kinase (DCk) and cytidine deaminase (CDA) were significantly down-regulated in drug-resistant cells (P<0.05). | |||
| Key Molecule: Deoxycytidine kinase (DCK) | [4] | |||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Jurkat cells | Pleural effusion | Homo sapiens (Human) | CVCL_0065 |
| Nalm-6 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0092 | |
| Experiment for Molecule Alteration |
Real-time quantitative PCR | |||
| Experiment for Drug Resistance |
CCK8 assay | |||
| Mechanism Description | Low-concentration cytarabine (Ara-C) continuously induced and cultured Jurkat and Nalm-6 cells to construct cytarabine-resistant cell lines Jurkat/Ara-C and Nalm-6/Ara-C. The results of real-time quantitative PCR showed that the expression of deoxycytidine kinase (DCk) and cytidine deaminase (CDA) were significantly down-regulated in drug-resistant cells (P<0.05). | |||
| Key Molecule: Cytidine deaminase (CDA) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Also opposing the activation pathway are the two deaminase CDA and deoxycytidine monophosphate deaminase (dCMPD). Cytidine deaminase is a multi-subunit enzyme involved in the maintenance of the pyrimidine nucleotide pool within the cell and physiologically catalyzes the hydrolytic deamination of cytidine to uridine and deoxycytidine to deoxyuridine. In cytarabine biotransformation, CDA removes the amine group from its cytosine and converts the drug into the inactive uracil arabinoside derivative. | |||
| Key Molecule: Cardiolipin synthase (CLS) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | CMPD deaminates cytarabine-monophosphate to arabinosyl-uracil-monophosphate. A crucial role for this latter enzyme has been suggested in the metabolism of cytarabine-monophosphate in T-lymphoblastic leukemia. | |||
| Key Molecule: Deoxycytidine kinase (DCK) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Deoxycitidine kinase plays a pivotal role since phosphorylation of cytarabine preserves intracellular retention of the drug and prevents from inactivation to its uridine derivative, uracil arabinoside, by cytidine deaminase. The intracellular accumulation of cytarabine triphosphate, the active cytotoxic metabolite, is proportional to the cellular DCk level which has led to the conclusion that DCk enzyme retains a rate-limiting role for the activation of cytarabine. | |||
| Key Molecule: UMP-CMP kinase (CMPK1) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Activation of cytarabine occurs by means of the step wise de novo synthesis of 5'-mono-, di-, and triphosphate derivatives throughout the sequential action of deoxycytidine kinase (DCk), deoxycytidine monophosphate kinase (dCMk), and nucleoside diphosphate kinase (NDk) encoded by the NME1 gene. Phosphorylated cytarabine metabolites interfere with the cellular pool of natural nucleosides, are incorporated into DNA and inhibit DNA synthesis in a competitive fashion. In vitro studies have revealed that the intracellular concentrations of cytarabine-triphosphate are higher in cytarabine sensitive cells than in resistant cells. | |||
| Key Molecule: Nucleoside diphosphate kinase A (NME1) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Activation of cytarabine occurs by means of the step wise de novo synthesis of 5'-mono-, di-, and triphosphate derivatives throughout the sequential action of deoxycytidine kinase (DCk), deoxycytidine monophosphate kinase (dCMk), and nucleoside diphosphate kinase (NDk) encoded by the NME1 gene. Phosphorylated cytarabine metabolites interfere with the cellular pool of natural nucleosides, are incorporated into DNA and inhibit DNA synthesis in a competitive fashion. In vitro studies have revealed that the intracellular concentrations of cytarabine-triphosphate are higher in cytarabine sensitive cells than in resistant cells. | |||
| Key Molecule: Cytosolic purine 5'-nucleotidase (NT5C2) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Since monophosphorilated intermediate of cytarabine activation is reduced by cytosolic 5'-nucleotidases NT5C2 and NT5C3, the activity level of this enzyme may represent one of the factors affecting the clinical outcome of cytarabine therapy. Increased expression of NT5C2 has been correlated with resistance to cytarabine chemotherapy and to a lower survival rate in a hundred patients undergoing cytarabine chemotherapy. An increase in the NT5C2 has emerged as a mechanism of resistance to cytarabine. Patients with AML and low expression level of NT5C2 have a better overall survival after treatment with cytarabine than patients with high expression. NT5C2 is implicated in pharmacokinetic of cytarabine has been associated with poor clinical outcome. | |||
|
|
||||
| Key Molecule: ATP-binding cassette sub-family C10 (ABCC10) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Uptake and accumulation of cytarabine is also regulated by transmembrane transporter proteins of the ABC family, also called human multidrug resistance-associated protein (MRP) family, namely ABCC10 (MRP7) and ABCC11 (MRP8) specifically committed to efflux of deoxynucleotides inactive metabolites and to temper intracellular pools of phosphorylated deoxynucleotides. The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Key Molecule: ATP-binding cassette sub-family C11(ABCC11) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Uptake and accumulation of cytarabine is also regulated by transmembrane transporter proteins of the ABC family, also called human multidrug resistance-associated protein (MRP) family, namely ABCC10 (MRP7) and ABCC11 (MRP8) specifically committed to efflux of deoxynucleotides inactive metabolites and to temper intracellular pools of phosphorylated deoxynucleotides. The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Key Molecule: Solute carrier family 29 member 1 (SLC29A1) | [2] | |||
| Resistant Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | Cytarabine gains entry into cells primarily as a false substrate through specialized nucleoside transporter proteins of SLC family, the human equilibrative nucleoside transportershENT1 and hENT2 (encoded by the gene SLC29A1 and SCL29A2, respectively) and the human concentrative nucleoside transporters hCNT3 (encoded by the gene SLC28A3). The drug accumulation may be substantially reduced when the expression of hENT1 transporter is deficient, or the activity of ABC drug efflux transporter proteins is elevated. | |||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: hsa-mir-181a | [16] | |||
| Sensitive Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| HL-60/Ara-C-resistant cells | Blood | Homo sapiens (Human) | CVCL_1736 | |
| Experiment for Molecule Alteration |
RT-PCR | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | Bcl-2 was conWrmed as adirect miR-181a target by immunoblot analysis andreporter gene assays. knockdown of Bcl-2 mimicked theeVect of enforced miR-181a expression by reducing cellviability. In addition, the apoptosis pathway was activated by cytochrome C release and caspase 9/caspase 3 activationafter miR-181a overexpression. Down-regulation of miR-181a and upregulation of Bcl-2in leukaemia cells confer resistance to Ara-C-based ther-apy. | |||
|
|
||||
| Key Molecule: Apoptosis regulator Bcl-2 (BCL2) | [16] | |||
| Sensitive Disease | Leukemia [ICD-11: 2B33.6] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | HL60 cells | Peripheral blood | Homo sapiens (Human) | CVCL_0002 |
| HL-60/Ara-C-resistant cells | Blood | Homo sapiens (Human) | CVCL_1736 | |
| Experiment for Molecule Alteration |
Western blot analysis | |||
| Experiment for Drug Resistance |
MTT assay | |||
| Mechanism Description | Bcl-2 was conWrmed as adirect miR-181a target by immunoblot analysis andreporter gene assays. knockdown of Bcl-2 mimicked theeVect of enforced miR-181a expression by reducing cellviability. In addition, the apoptosis pathway was activated by cytochrome C release and caspase 9/caspase 3 activationafter miR-181a overexpression. Down-regulation of miR-181a and upregulation of Bcl-2in leukaemia cells confer resistance to Ara-C-based ther-apy. | |||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
