Molecule Information
General Information of the Molecule (ID: Mol00006)
| Name |
Tyrosine-protein kinase ABL1 (ABL1)
,Homo sapiens
|
||||
|---|---|---|---|---|---|
| Synonyms |
Abelson murine leukemia viral oncogene homolog 1; Abelson tyrosine-protein kinase 1; Proto-oncogene c-Abl; p150; ABL; JTK7
Click to Show/Hide
|
||||
| Molecule Type |
Protein
|
||||
| Gene Name |
ABL1
|
||||
| Gene ID | |||||
| Location |
chr9:130713016-130887675[+]
|
||||
| Sequence |
MLEICLKLVGCKSKKGLSSSSSCYLEEALQRPVASDFEPQGLSEAARWNSKENLLAGPSE
NDPNLFVALYDFVASGDNTLSITKGEKLRVLGYNHNGEWCEAQTKNGQGWVPSNYITPVN SLEKHSWYHGPVSRNAAEYLLSSGINGSFLVRESESSPGQRSISLRYEGRVYHYRINTAS DGKLYVSSESRFNTLAELVHHHSTVADGLITTLHYPAPKRNKPTVYGVSPNYDKWEMERT DITMKHKLGGGQYGEVYEGVWKKYSLTVAVKTLKEDTMEVEEFLKEAAVMKEIKHPNLVQ LLGVCTREPPFYIITEFMTYGNLLDYLRECNRQEVNAVVLLYMATQISSAMEYLEKKNFI HRDLAARNCLVGENHLVKVADFGLSRLMTGDTYTAHAGAKFPIKWTAPESLAYNKFSIKS DVWAFGVLLWEIATYGMSPYPGIDLSQVYELLEKDYRMERPEGCPEKVYELMRACWQWNP SDRPSFAEIHQAFETMFQESSISDEVEKELGKQGVRGAVSTLLQAPELPTKTRTSRRAAE HRDTTDVPEMPHSKGQGESDPLDHEPAVSPLLPRKERGPPEGGLNEDERLLPKDKKTNLF SALIKKKKKTAPTPPKRSSSFREMDGQPERRGAGEEEGRDISNGALAFTPLDTADPAKSP KPSNGAGVPNGALRESGGSGFRSPHLWKKSSTLTSSRLATGEEEGGGSSSKRFLRSCSAS CVPHGAKDTEWRSVTLPRDLQSTGRQFDSSTFGGHKSEKPALPRKRAGENRSDQVTRGTV TPPPRLVKKNEEAADEVFKDIMESSPGSSPPNLTPKPLRRQVTVAPASGLPHKEEAGKGS ALGTPAAAEPVTPTSKAGSGAPGGTSKGPAEESRVRRHKHSSESPGRDKGKLSRLKPAPP PPPAASAGKAGGKPSQSPSQEAAGEAVLGAKTKATSLVDAVNSDAAKPSQPGEGLKKPVL PATPKPQSAKPSGTPISPAPVPSTLPSASSALAGDQPSSTAFIPLISTRVSLRKTRQPPE RIASGAITKGVVLDSTEALCLAISRNSEQMASHSAVLEAGKNLYTFCVSYVDSIQQMRNK FAFREAINKLENNLRELQICPATAGSGPAATQDFSKLLSSVKEISDIVQR Click to Show/Hide
|
||||
| 3D-structure |
|
||||
| Function |
Non-receptor tyrosine-protein kinase that plays a role in many key processes linked to cell growth and survival such as cytoskeleton remodeling in response to extracellular stimuli, cell motility and adhesion, receptor endocytosis, autophagy, DNA damage response and apoptosis. Coordinates actin remodeling through tyrosine phosphorylation of proteins controlling cytoskeleton dynamics like WASF3 (involved in branch formation); ANXA1 (involved in membrane anchoring); DBN1, DBNL, CTTN, RAPH1 and ENAH (involved in signaling); or MAPT and PXN (microtubule-binding proteins). Phosphorylation of WASF3 is critical for the stimulation of lamellipodia formation and cell migration. Involved in the regulation of cell adhesion and motility through phosphorylation of key regulators of these processes such as BCAR1, CRK, CRKL, DOK1, EFS or NEDD9. Phosphorylates multiple receptor tyrosine kinases and more particularly promotes endocytosis of EGFR, facilitates the formation of neuromuscular synapses through MUSK, inhibits PDGFRB-mediated chemotaxis and modulates the endocytosis of activated B-cell receptor complexes. Other substrates which are involved in endocytosis regulation are the caveolin (CAV1) and RIN1. Moreover, ABL1 regulates the CBL family of ubiquitin ligases that drive receptor down-regulation and actin remodeling. Phosphorylation of CBL leads to increased EGFR stability. Involved in late-stage autophagy by regulating positively the trafficking and function of lysosomal components. ABL1 targets to mitochondria in response to oxidative stress and thereby mediates mitochondrial dysfunction and cell death. In response to oxidative stress, phosphorylates serine/threonine kinase PRKD2 at 'Tyr-717'. ABL1 is also translocated in the nucleus where it has DNA-binding activity and is involved in DNA-damage response and apoptosis. Many substrates are known mediators of DNA repair: DDB1, DDB2, ERCC3, ERCC6, RAD9A, RAD51, RAD52 or WRN. Activates the proapoptotic pathway when the DNA damage is too severe to be repaired. Phosphorylates TP73, a primary regulator for this type of damage-induced apoptosis. Phosphorylates the caspase CASP9 on 'Tyr-153' and regulates its processing in the apoptotic response to DNA damage. Phosphorylates PSMA7 that leads to an inhibition of proteasomal activity and cell cycle transition blocks. ABL1 acts also as a regulator of multiple pathological signaling cascades during infection. Several known tyrosine-phosphorylated microbial proteins have been identified as ABL1 substrates. This is the case of A36R of Vaccinia virus, Tir (translocated intimin receptor) of pathogenic E.coli and possibly Citrobacter, CagA (cytotoxin-associated gene A) of H.pylori, or AnkA (ankyrin repeat-containing protein A) of A.phagocytophilum. Pathogens can highjack ABL1 kinase signaling to reorganize the host actin cytoskeleton for multiple purposes, like facilitating intracellular movement and host cell exit. Finally, functions as its own regulator through autocatalytic activity as well as through phosphorylation of its inhibitor, ABI1. Regulates T-cell differentiation in a TBX21-dependent manner. Phosphorylates TBX21 on tyrosine residues leading to an enhancement of its transcriptional activator activity.
Click to Show/Hide
|
||||
| Uniprot ID | |||||
| Ensembl ID | |||||
| HGNC ID | |||||
| Click to Show/Hide the Complete Species Lineage | |||||
Type(s) of Resistant Mechanism of This Molecule
Drug Resistance Data Categorized by Drug
Approved Drug(s)
8 drug(s) in total
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Non-small cell lung cancer [ICD-11: 2C25.Y] | [1] | ||||||||||||
| Resistant Disease | Non-small cell lung cancer [ICD-11: 2C25.Y] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Expression | Down-regulation |
|||||||||||
| Differential expression of the molecule in resistant disease | |||||||||||||
| Classification of Disease | Lung cancer [ICD-11: 2C25] | ||||||||||||
| The Specified Disease | Non-small cell lung cancer | ||||||||||||
| The Studied Tissue | Lung tissue | ||||||||||||
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.17E-11 Fold-change: -1.61E-01 Z-score: -7.19E+00 |
||||||||||||
| Experimental Note | Revealed Based on the Cell Line Data | ||||||||||||
| Cell Pathway Regulation | Abl/RAS/ERK signaling pathway | Activation | hsa04010 | ||||||||||
| Cell proliferation | Activation | hsa05200 | |||||||||||
| In Vitro Model | H292 cells | Lung | Homo sapiens (Human) | CVCL_0455 | |||||||||
| A549 cells | Lung | Homo sapiens (Human) | CVCL_0023 | ||||||||||
| In Vivo Model | Nude mouse xenograft model | Mus musculus | |||||||||||
| Experiment for Molecule Alteration |
Western blot analysis | ||||||||||||
| Experiment for Drug Resistance |
CCK8 assay | ||||||||||||
| Mechanism Description | Reduced miR-3127-5p expression promotes NSCLC proliferation/invasion and contributes to dasatinib sensitivity via the c-Abl/Ras/ERk pathway. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [14] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Expression | Up-regulation |
|||||||||||
| Experimental Note | Revealed Based on the Cell Line Data | ||||||||||||
| Cell Pathway Regulation | Cell apoptosis | Inhibition | hsa04210 | ||||||||||
| Cell proliferation | Activation | hsa05200 | |||||||||||
| In Vitro Model | K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |||||||||
| Ku812 cells | Bone marrow | Homo sapiens (Human) | CVCL_0379 | ||||||||||
| Experiment for Molecule Alteration |
Western blot analysis; qRT-PCR | ||||||||||||
| Experiment for Drug Resistance |
CCk reagent assay; Flow cytometry assay | ||||||||||||
| Mechanism Description | CircBA9.3 promoted cell proliferation and reduced the sensitivity of leukaemic cells to TkIs through up-regulation of the ABL1 and BCR-ABL1 protein expression levels. | ||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [3], [6], [7] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [8], [9] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Drug Resistance |
Flow cytometry assay; Analysis of disease free and overall survival assay | ||||||||||||
| Mechanism Description | Mutations were frequently detected at relapse. Among 17 patients analyzed, a T315I mutation was detected in 12, E255k in 1, and no BCR-ABL mutations in 4 (25886620). Thirteen relapsed patients had mutational analysis and 7 had ABL mutations (4 T315I, 1 F359V, and 2 V299L). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [7], [10] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G250E |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Mutant Type Structure | Method: Solution NMR | Resolution: N.A. | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
60
|
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
-
R
-
70
|
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
-
G
-
80
|
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
-
K
-
90
|
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
-
N
-
100
|
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
-
D
-
110
|
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
-
S
-
120
|
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
-
L
-
130
|
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
-
E
-
140
|
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
-
V
-
150
|
P
-
S
-
N
-
Y
-
I
-
T
-
P
-
V
-
N
-
S
-
160
|
L
-
E
-
K
-
H
-
S
-
W
-
Y
-
H
-
G
-
P
-
170
|
V
-
S
-
R
-
N
-
A
-
A
-
E
-
Y
-
L
-
L
-
180
|
S
-
S
-
G
-
I
-
N
-
G
-
S
-
F
-
L
-
V
-
190
|
R
-
E
-
S
-
E
-
S
-
S
-
P
-
G
-
Q
-
R
-
200
|
S
-
I
-
S
-
L
-
R
-
Y
-
E
-
G
-
R
-
V
-
210
|
Y
-
H
-
Y
-
R
-
I
-
N
-
T
-
A
-
S
-
D
-
220
|
G
-
K
-
L
-
Y
-
V
-
S
-
S
-
E
-
S
-
R
-
230
|
F
-
N
-
T
-
L
-
A
-
E
-
L
-
V
-
H
-
H
-
240
|
H
-
S
-
T
-
V
-
A
-
D
-
G
-
L
-
I
-
T
-
250
|
T
-
L
-
H
-
Y
-
P
-
A
-
P
-
K
-
R
-
N
-
260
|
K
-
P
-
T
-
V
-
Y
-
G
-
V
-
S
S
P
P
N
N
270
|
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
D
D
280
|
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
E
G
G
290
|
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
W
W
300
|
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
K
K
310
|
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
E
E
320
|
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
L
K
K
330
|
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
L
L
340
|
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
F
F
350
|
Y
Y
I
I
I
I
I
T
E
E
F
F
M
M
T
T
Y
Y
G
G
360
|
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
N
N
370
|
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
L
L
380
|
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
M
M
390
|
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
H
H
400
|
R
R
N
D
L
L
A
A
A
A
R
R
N
N
C
C
L
L
V
V
410
|
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
D
D
420
|
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
Y
G
G
D
D
430
|
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
F
F
440
|
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
L
L
450
|
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
D
D
460
|
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
E
E
470
|
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
P
P
480
|
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
L
L
490
|
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
P
P
500
|
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
L
L
510
|
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
S
S
520
|
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
Q
Q
530
|
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
S
S
540
|
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
G
G
550
|
K
K
Q
Q
G
G
V
V
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [3], [6], [7] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V338F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [10], [12] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V299L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V268A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [4], [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Q252H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M351T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M244V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L387M |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L384M |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L298V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L248V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.H396R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F311L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E459K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E355G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence 23223358. We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D325G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [8] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Drug Resistance |
Flow cytometry assay | ||||||||||||
| Mechanism Description | Mutations were frequently detected at relapse. Among 17 patients analyzed, a T315I mutation was detected in 12, E255k in 1, and no BCR-ABL mutations in 4. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [10] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T495R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Mechanism Description | The most common mechanism of acquired resistance in CML in imatinib era is the acquisition of BCR-ABL kinase domain mutations with decreased sensitivity to the drug. Our findings demonstrate the potential hazards of sequential kinase inhibitor therapy and suggest a role for a combination of ABL kinase inhibitors, perhaps including drugs with different mechanisms of action, to prevent the outgrowth of cells harboring drug-resistant BCR-ABL mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M388L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
RNA sequencing assay | ||||||||||||
| Mechanism Description | The presence of BCR-ABL oncogene mutations in patients with chronic myeloid leukemia (CML) may be responsible for the failure of tyrosine kinase inhibitor (TkI) treatment. In addition to 9 point mutations (G250E / F317L, F359V, L387M, Y253H, M388L, M244V, T315I, D276G), 35 bp insertion between exons 8 and 9 and deletion exon 7 were detected. Our results demonstrate that direct sequencing is suitable for routine clinical monitoring patients with CML and may be useful for optimizing therapy. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [9] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V299L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Drug Resistance |
Analysis of disease free and overall survival assay | ||||||||||||
| Mechanism Description | Thirteen relapsed patients had mutational analysis and 7 had ABL mutations (4 T315I, 1 F359V, and 2 V299L). | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [9] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Drug Resistance |
Analysis of disease free and overall survival assay | ||||||||||||
| Mechanism Description | Thirteen relapsed patients had mutational analysis and 7 had ABL mutations (4 T315I, 1 F359V, and 2 V299L). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y353H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V379I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L273M |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Disease Class: Acute T-cell lymphocytic leukemia [ICD-11: 2A90.5] | [4] | ||||||||||||
| Resistant Disease | Acute T-cell lymphocytic leukemia [ICD-11: 2A90.5] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Tritiated thymidine incorporation assay | ||||||||||||
| Mechanism Description | Mutations may impair TkI activity by directly or indirectly impairing the drug binding to the protein. We report the discovery of three new BCR/ABL mutations, L248R, T315V, and F317R identified in two patients with CML (L248R and T315V) and in one patient with Ph+ acute lymphoblastic leukemia (ALL) (F317R). | ||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Dasatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D444Y |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Solid tumour/cancer [ICD-11: 2A00-2F9Z] | [2] | ||||||||||||
| Sensitive Disease | Solid tumour/cancer [ICD-11: 2A00-2F9Z] | ||||||||||||
| Sensitive Drug | Axitinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I (c.944C>T) |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Bone marrow | N.A. | |||||||||||
| Mechanism Description | The missense mutation p.T315I (c.944C>T) in gene ABL1 cause the sensitivity of Axitinib by aberration of the drug's therapeutic target | ||||||||||||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [3] | |||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | |||
| Resistant Drug | Bosutinib | |||
| Molecule Alteration | Missense mutation | p.F359V |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | ||
| Experiment for Molecule Alteration |
Direct sequencing assay | |||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | |||
| Mechanism Description | Patients with more than one BCR-ABL1 mutation fare worse than those with no or one mutation. | |||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [3] | |||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | |||
| Resistant Drug | Bosutinib | |||
| Molecule Alteration | Missense mutation | p.M351T |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | ||
| Experiment for Molecule Alteration |
Direct sequencing assay | |||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | |||
| Mechanism Description | Patients with more than one BCR-ABL1 mutation fare worse than those with no or one mutation. | |||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [4] | |||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | |||
| Resistant Drug | Bosutinib | |||
| Molecule Alteration | Missense mutation | p.F359I |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Experiment for Molecule Alteration |
Direct sequencing assay | |||
| Experiment for Drug Resistance |
Tritiated thymidine incorporation assay | |||
| Mechanism Description | L248R was identified in a patient with lymphoid Blast Crisis (BC) CML (Patient no. 1), in cis with a pre-existing mutation. The patient initially presented with an imatinib-resistant F359I mutation. | |||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [4] | |||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | |||
| Resistant Drug | Bosutinib | |||
| Molecule Alteration | Missense mutation | p.L248R |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Experiment for Molecule Alteration |
Direct sequencing assay | |||
| Experiment for Drug Resistance |
Tritiated thymidine incorporation assay | |||
| Mechanism Description | Mutations may impair TkI activity by directly or indirectly impairing the drug binding to the protein. We report the discovery of three new BCR/ABL mutations, L248R, T315V, and F317R identified in two patients with CML (L248R and T315V) and in one patient with Ph+ acute lymphoblastic leukemia (ALL) (F317R). | |||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Disease Class: Solid tumour/cancer [ICD-11: 2A00-2F9Z] | [5] | |||
| Sensitive Disease | Solid tumour/cancer [ICD-11: 2A00-2F9Z] | |||
| Sensitive Drug | Cabozantinib | |||
| Molecule Alteration | Missense mutation | p.V299L (c.895G>C) |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Ba/F3 cells | Colon | Homo sapiens (Human) | CVCL_0161 |
| Ph+ALL cells | N.A. | N.A. | N.A. | |
| Mechanism Description | The missense mutation p.V299L (c.895G>C) in gene ABL1 cause the sensitivity of Cabozantinib by aberration of the drug's therapeutic target | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15], [16] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.H396P |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.20 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.00 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
S
-
S
-
230
|
P
-
N
-
Y
-
D
-
K
-
W
-
E
-
M
-
E
-
R
-
240
|
T
-
D
-
I
-
T
-
M
-
K
G
H
H
K
M
L
S
G
P
250
|
G
N
G
Y
Q
D
Y
K
G
W
E
E
V
M
Y
E
E
R
G
T
260
|
V
D
W
I
K
T
K
M
Y
K
S
H
L
K
T
L
V
G
A
G
270
|
V
G
K
Q
T
Y
L
G
K
E
E
V
D
Y
T
E
M
G
E
V
280
|
V
W
E
K
E
K
F
Y
L
S
K
L
E
T
A
V
A
A
V
V
290
|
M
K
K
T
E
L
I
K
K
E
H
D
P
T
N
M
L
E
V
V
300
|
Q
E
L
E
L
F
G
L
V
K
C
E
T
A
R
A
E
V
P
M
310
|
P
K
F
E
Y
I
I
K
I
H
T
P
E
N
F
L
M
V
T
Q
320
|
Y
L
G
L
N
G
L
V
L
C
D
T
Y
R
L
E
R
P
E
P
330
|
C
F
N
Y
R
I
Q
I
E
T
V
E
N
F
A
M
V
T
V
Y
340
|
L
G
L
N
Y
L
M
L
A
D
T
Y
Q
L
I
R
S
E
S
C
350
|
A
N
M
R
E
Q
Y
E
L
V
E
N
K
A
K
V
N
V
F
L
360
|
I
L
H
Y
R
M
D
A
L
T
A
Q
A
I
R
S
N
S
C
A
370
|
L
M
V
E
G
Y
E
L
N
E
H
K
L
K
V
N
K
F
V
I
380
|
A
H
D
R
F
D
G
L
L
A
S
A
R
R
L
N
M
C
T
L
390
|
G
V
D
G
T
E
Y
N
T
H
A
L
H
V
A
K
G
V
A
A
400
|
K
D
F
F
P
G
I
L
K
S
W
R
T
L
A
M
P
T
E
G
410
|
S
D
L
T
A
Y
Y
T
N
A
K
P
F
A
S
G
I
A
K
K
420
|
S
F
D
P
V
I
W
K
A
W
F
T
G
A
V
P
L
E
L
S
430
|
W
L
E
A
I
Y
A
N
T
K
Y
F
G
S
M
I
S
K
P
S
440
|
Y
D
P
V
G
W
I
A
D
F
L
G
S
V
Q
L
V
L
Y
W
450
|
E
E
L
I
L
A
E
T
K
Y
D
G
Y
M
R
S
M
P
E
Y
460
|
R
P
P
G
E
I
G
D
C
L
P
S
E
Q
K
V
V
Y
Y
E
470
|
E
L
L
L
M
E
R
K
A
D
C
Y
W
R
Q
M
W
E
N
R
480
|
P
P
S
E
D
G
R
C
P
P
S
E
F
K
A
V
E
Y
I
E
490
|
H
L
Q
M
A
R
F
A
E
C
T
W
M
Q
F
W
Q
N
E
P
500
|
S
S
S
D
I
R
S
P
D
S
E
F
V
A
E
E
K
I
E
H
510
|
L
Q
G
A
K
F
-
E
-
T
-
M
-
F
-
Q
-
E
-
S
520
|
-
S
-
I
-
S
-
D
-
E
-
V
-
E
-
K
-
E
-
L
530
|
-
G
-
K
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Pyrosequencing analysis | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Imatinib resistance in chronic myeloid leukemia (CML) is commonly due to BCR-ABL kinase domain mutations (kDMs). | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [17], [18] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.H396P |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.20 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.00 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
S
-
S
-
230
|
P
-
N
-
Y
-
D
-
K
-
W
-
E
-
M
-
E
-
R
-
240
|
T
-
D
-
I
-
T
-
M
-
K
G
H
H
K
M
L
S
G
P
250
|
G
N
G
Y
Q
D
Y
K
G
W
E
E
V
M
Y
E
E
R
G
T
260
|
V
D
W
I
K
T
K
M
Y
K
S
H
L
K
T
L
V
G
A
G
270
|
V
G
K
Q
T
Y
L
G
K
E
E
V
D
Y
T
E
M
G
E
V
280
|
V
W
E
K
E
K
F
Y
L
S
K
L
E
T
A
V
A
A
V
V
290
|
M
K
K
T
E
L
I
K
K
E
H
D
P
T
N
M
L
E
V
V
300
|
Q
E
L
E
L
F
G
L
V
K
C
E
T
A
R
A
E
V
P
M
310
|
P
K
F
E
Y
I
I
K
I
H
T
P
E
N
F
L
M
V
T
Q
320
|
Y
L
G
L
N
G
L
V
L
C
D
T
Y
R
L
E
R
P
E
P
330
|
C
F
N
Y
R
I
Q
I
E
T
V
E
N
F
A
M
V
T
V
Y
340
|
L
G
L
N
Y
L
M
L
A
D
T
Y
Q
L
I
R
S
E
S
C
350
|
A
N
M
R
E
Q
Y
E
L
V
E
N
K
A
K
V
N
V
F
L
360
|
I
L
H
Y
R
M
D
A
L
T
A
Q
A
I
R
S
N
S
C
A
370
|
L
M
V
E
G
Y
E
L
N
E
H
K
L
K
V
N
K
F
V
I
380
|
A
H
D
R
F
D
G
L
L
A
S
A
R
R
L
N
M
C
T
L
390
|
G
V
D
G
T
E
Y
N
T
H
A
L
H
V
A
K
G
V
A
A
400
|
K
D
F
F
P
G
I
L
K
S
W
R
T
L
A
M
P
T
E
G
410
|
S
D
L
T
A
Y
Y
T
N
A
K
P
F
A
S
G
I
A
K
K
420
|
S
F
D
P
V
I
W
K
A
W
F
T
G
A
V
P
L
E
L
S
430
|
W
L
E
A
I
Y
A
N
T
K
Y
F
G
S
M
I
S
K
P
S
440
|
Y
D
P
V
G
W
I
A
D
F
L
G
S
V
Q
L
V
L
Y
W
450
|
E
E
L
I
L
A
E
T
K
Y
D
G
Y
M
R
S
M
P
E
Y
460
|
R
P
P
G
E
I
G
D
C
L
P
S
E
Q
K
V
V
Y
Y
E
470
|
E
L
L
L
M
E
R
K
A
D
C
Y
W
R
Q
M
W
E
N
R
480
|
P
P
S
E
D
G
R
C
P
P
S
E
F
K
A
V
E
Y
I
E
490
|
H
L
Q
M
A
R
F
A
E
C
T
W
M
Q
F
W
Q
N
E
P
500
|
S
S
S
D
I
R
S
P
D
S
E
F
V
A
E
E
K
I
E
H
510
|
L
Q
G
A
K
F
-
E
-
T
-
M
-
F
-
Q
-
E
-
S
520
|
-
S
-
I
-
S
-
D
-
E
-
V
-
E
-
K
-
E
-
L
530
|
-
G
-
K
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
CR-Abl sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay | ||||||||||||
| Mechanism Description | M244V and H396 mutations have been shown to be more resistant to imatinib but both have been shown to be sensitive to second generation TkI's such as nilotinib and dasatinib. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [17] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Mechanism Description | Different mutations within the kinase domain of BCR-ABL can be responsible for refractoriness of Ph+ leukaemia to STI571. Mutation in the BCR-ABL kinase domain might be a frequent mechanism of STI571 resistance in lymphoid disease. In summary, binding of STI571 to BCR-ABL depends on a number of specific interactions within the ATPbinding site. Our results strongly suggest that a patient could be resistant to STI571 by acquisition of different individual point mutations within the ATP-binding pocket or activation loop of BCR-ABL, even though the number of mutations might be limited. This factor could make it difficult to overcome resistance to STI571 by use of alternative kinase inhibitors. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [19], [20], [21] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G250E |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Mutant Type Structure | Method: Solution NMR | Resolution: N.A. | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
60
|
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
-
R
-
70
|
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
-
G
-
80
|
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
-
K
-
90
|
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
-
N
-
100
|
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
-
D
-
110
|
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
-
S
-
120
|
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
-
L
-
130
|
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
-
E
-
140
|
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
-
V
-
150
|
P
-
S
-
N
-
Y
-
I
-
T
-
P
-
V
-
N
-
S
-
160
|
L
-
E
-
K
-
H
-
S
-
W
-
Y
-
H
-
G
-
P
-
170
|
V
-
S
-
R
-
N
-
A
-
A
-
E
-
Y
-
L
-
L
-
180
|
S
-
S
-
G
-
I
-
N
-
G
-
S
-
F
-
L
-
V
-
190
|
R
-
E
-
S
-
E
-
S
-
S
-
P
-
G
-
Q
-
R
-
200
|
S
-
I
-
S
-
L
-
R
-
Y
-
E
-
G
-
R
-
V
-
210
|
Y
-
H
-
Y
-
R
-
I
-
N
-
T
-
A
-
S
-
D
-
220
|
G
-
K
-
L
-
Y
-
V
-
S
-
S
-
E
-
S
-
R
-
230
|
F
-
N
-
T
-
L
-
A
-
E
-
L
-
V
-
H
-
H
-
240
|
H
-
S
-
T
-
V
-
A
-
D
-
G
-
L
-
I
-
T
-
250
|
T
-
L
-
H
-
Y
-
P
-
A
-
P
-
K
-
R
-
N
-
260
|
K
-
P
-
T
-
V
-
Y
-
G
-
V
-
S
S
P
P
N
N
270
|
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
D
D
280
|
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
E
G
G
290
|
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
W
W
300
|
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
K
K
310
|
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
E
E
320
|
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
L
K
K
330
|
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
L
L
340
|
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
F
F
350
|
Y
Y
I
I
I
I
I
T
E
E
F
F
M
M
T
T
Y
Y
G
G
360
|
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
N
N
370
|
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
L
L
380
|
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
M
M
390
|
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
H
H
400
|
R
R
N
D
L
L
A
A
A
A
R
R
N
N
C
C
L
L
V
V
410
|
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
D
D
420
|
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
Y
G
G
D
D
430
|
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
F
F
440
|
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
L
L
450
|
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
D
D
460
|
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
E
E
470
|
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
P
P
480
|
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
L
L
490
|
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
P
P
500
|
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
L
L
510
|
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
S
S
520
|
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
Q
Q
530
|
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
S
S
540
|
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
G
G
550
|
K
K
Q
Q
G
G
V
V
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [22] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G250E |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Mutant Type Structure | Method: Solution NMR | Resolution: N.A. | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
60
|
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
-
R
-
70
|
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
-
G
-
80
|
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
-
K
-
90
|
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
-
N
-
100
|
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
-
D
-
110
|
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
-
S
-
120
|
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
-
L
-
130
|
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
-
E
-
140
|
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
-
V
-
150
|
P
-
S
-
N
-
Y
-
I
-
T
-
P
-
V
-
N
-
S
-
160
|
L
-
E
-
K
-
H
-
S
-
W
-
Y
-
H
-
G
-
P
-
170
|
V
-
S
-
R
-
N
-
A
-
A
-
E
-
Y
-
L
-
L
-
180
|
S
-
S
-
G
-
I
-
N
-
G
-
S
-
F
-
L
-
V
-
190
|
R
-
E
-
S
-
E
-
S
-
S
-
P
-
G
-
Q
-
R
-
200
|
S
-
I
-
S
-
L
-
R
-
Y
-
E
-
G
-
R
-
V
-
210
|
Y
-
H
-
Y
-
R
-
I
-
N
-
T
-
A
-
S
-
D
-
220
|
G
-
K
-
L
-
Y
-
V
-
S
-
S
-
E
-
S
-
R
-
230
|
F
-
N
-
T
-
L
-
A
-
E
-
L
-
V
-
H
-
H
-
240
|
H
-
S
-
T
-
V
-
A
-
D
-
G
-
L
-
I
-
T
-
250
|
T
-
L
-
H
-
Y
-
P
-
A
-
P
-
K
-
R
-
N
-
260
|
K
-
P
-
T
-
V
-
Y
-
G
-
V
-
S
S
P
P
N
N
270
|
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
D
D
280
|
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
E
G
G
290
|
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
W
W
300
|
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
K
K
310
|
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
E
E
320
|
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
L
K
K
330
|
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
L
L
340
|
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
F
F
350
|
Y
Y
I
I
I
I
I
T
E
E
F
F
M
M
T
T
Y
Y
G
G
360
|
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
N
N
370
|
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
L
L
380
|
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
M
M
390
|
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
H
H
400
|
R
R
N
D
L
L
A
A
A
A
R
R
N
N
C
C
L
L
V
V
410
|
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
D
D
420
|
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
Y
G
G
D
D
430
|
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
F
F
440
|
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
L
L
450
|
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
D
D
460
|
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
E
E
470
|
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
P
P
480
|
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
L
L
490
|
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
P
P
500
|
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
L
L
510
|
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
S
S
520
|
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
Q
Q
530
|
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
S
S
540
|
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
G
G
550
|
K
K
Q
Q
G
G
V
V
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
PCR-Invader assay; Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | The PCR-Invader assay used in this study is an appropriate tool for the screening of mutations during TkI therapy. High Sokal score is only predictive factor for emergence of mutation in CML-CP. P-loop mutations were associated with poor PFS in CML-CP. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253H+p.F317L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I+p.E459K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.P480L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M244V+p.G250E |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [24], [25], [26] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E459K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E450K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [23] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K+p.T315I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [17], [19], [20] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Among the 32 patients with baseline mutation, mutations including M244V, G250E, E255k, M351T, H396R, S417Y, E450k and E459k disappeared in 8 patients and new mutations were detected in 9 patients, all of which were T315I. Among the 23 patients without baseline mutation, 4 patients showed newly developed mutations including T315I, T315I + E459k, M244V and F359V. The T315I was the most frequently detected mutation in imatinib therapy (16%, 9 of 55) as well as in dasatinib or nilotinib therapy (24%, 11 of 44). Patients with imatinib resistant baseline mutations had a higher rate of mutation development during dasatinib or nilotinib treatment compared to patients without baseline mutations (28% vs. 17%). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y320C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [27], [28] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V299L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V256L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27], [29] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T277A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.S438C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M351K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.K378R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E494G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15], [27], [30] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E450G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E355G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [27] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.A399T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay; Event-free survival (EFS) assay | ||||||||||||
| Mechanism Description | Compared to non-mutated patients, subjects with point mutations had a worse response to dasatinib, with significantly lower rates of complete cytogenetic response (57 vs 32 %), higher percentage of primary resistance (16/36 vs 6/40) and a trend towards a shorter median event-free survival. In elderly patients, the presence of a mutation at the time of imatinib failure is associated with a worse response to dasatinib therapy. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [17] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Mechanism Description | Different mutations within the kinase domain of BCR-ABL can be responsible for refractoriness of Ph+ leukaemia to STI571. Mutation in the BCR-ABL kinase domain might be a frequent mechanism of STI571 resistance in lymphoid disease. In summary, binding of STI571 to BCR-ABL depends on a number of specific interactions within the ATPbinding site. Our results strongly suggest that a patient could be resistant to STI571 by acquisition of different individual point mutations within the ATP-binding pocket or activation loop of BCR-ABL, even though the number of mutations might be limited. This factor could make it difficult to overcome resistance to STI571 by use of alternative kinase inhibitors. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [31] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.N368S |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Denaturing high performance liquid chromatography (dHPLC) assay; Direct DNA sequencing method assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay | ||||||||||||
| Mechanism Description | Fifteen different types of mutations (T315I, E255k, G250E, M351T, F359C, G251E, Y253H, V289F, E355G, N368S, L387M, H369R, A397P, E355A, D276G), including 2 novel mutations were identified, with T315I as the predominant type of mutation. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [31] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G251E |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Denaturing high performance liquid chromatography (dHPLC) assay; Direct DNA sequencing method assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay | ||||||||||||
| Mechanism Description | Fifteen different types of mutations (T315I, E255k, G250E, M351T, F359C, G251E, Y253H, V289F, E355G, N368S, L387M, H369R, A397P, E355A, D276G), including 2 novel mutations were identified, with T315I as the predominant type of mutation. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [31], [32], [33] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.A397P |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Denaturing high performance liquid chromatography (dHPLC) assay; Direct DNA sequencing method assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay | ||||||||||||
| Mechanism Description | Fifteen different types of mutations (T315I, E255k, G250E, M351T, F359C, G251E, Y253H, V289F, E355G, N368S, L387M, H369R, A397P, E355A, D276G), including 2 novel mutations were identified, with T315I as the predominant type of mutation. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V338F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V268A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26], [32], [33] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L298V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15], [23], [26] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [11] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D325G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Sanger sequencing assay | ||||||||||||
| Mechanism Description | For CML patients on TkI therapy, 70% of double mutations in the BCR-ABL1 kinase domain detected by direct sequencing are compound mutations. Sequential, branching, and parallel routes to compound mutations were observed, suggesting complex patterns of emergence. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [34] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Q252K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Next generation sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | HSCT is an important salvage option for TkI-resistant patients with or without BCR-ABL1 mutations. Patients with mutations were more likely to develop advanced disease and had worse outcomes after HSCT. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [19], [20], [21] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F311I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
PCR-Invader assay; Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | The PCR-Invader assay used in this study is an appropriate tool for the screening of mutations during TkI therapy. High Sokal score is only predictive factor for emergence of mutation in CML-CP. P-loop mutations were associated with poor PFS in CML-CP. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [35] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Q252E |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | In late CP or advanced CML, ABL-kinase mutations occur as an intraclonal event in the primitive Ph1+ stem cell compartments with progression of this clone towards IM-resistant blast phase. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [36] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Denaturing high-power liquid chromatography assay | ||||||||||||
| Mechanism Description | Our results confirm the high frequency of BCR-ABL kinase domain mutations in patients with secondary resistance to imatinib and exclude mutations of the activation loops of kIT, PDGFRA and PDGFRB as possible causes of resistance in patients without ABL mutations. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [36] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D276G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Denaturing high-power liquid chromatography assay | ||||||||||||
| Mechanism Description | Our results confirm the high frequency of BCR-ABL kinase domain mutations in patients with secondary resistance to imatinib and exclude mutations of the activation loops of kIT, PDGFRA and PDGFRB as possible causes of resistance in patients without ABL mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15], [26], [37] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L364I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Real-time Taqman assay; Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay | ||||||||||||
| Mechanism Description | Point mutation was the major mechanism of primary cytogenetic resistance to imatinib mesylate in the present study. Patients with mutations had inferior progression-free survival compared to those without mutations. Resistance is higher among patients with advanced CML. Point mutations in the ABL kinase domain and amplification of the BCR-ABL fusion gene have emerged as important mechanisms responsible for resistance to imatinib. Biochemical and cellular assays have demonstrated that different BCR-ABL mutations might result in varying levels of resistance. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [31], [38], [39] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.V289F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Overall survival assay | ||||||||||||
| Mechanism Description | Point mutations were detected in 36 of 154 patients by direct sequencing. In our series, the single most common mutations were G250E, E255k/V, and M351T. The presence of mutations correlated significantly with accelerated phase, lack of molecular response, and lower cytogenetic and hematological responses. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [19] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Point mutations were found in the adenosine triphosphate (ATP) binding region of BCR/ABL in 12 of 18 patients with chronic myeloid leukemia (CML) or Ph-positive acute lymphoblastic leukemia (Ph+ ALL) and imatinib resistance (defined as loss of established hematologic response). Three mutations (T315I, Y253H, and F317L present in 3, 1, and 1 patients, respectively) have a predicted role in abrogating imatinib binding to BCR/ABL, whereas 3 other mutations (E255k, G250E, and M351T, present in 4, 2, and 2 patients, respectively) do not. Thus we confirm a high frequency of mutations clustered within the ATP-binding region of BCR/ABL in resistant patients. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [15], [40] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L273M |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [41] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.N374Y |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Nested RT-PC assay; Gene sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Presence of mutations predicted for poorer responses and EFS to dose escalation. IM dose escalation is likely to be effective only in those harboring no or relatively sensitive kD mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [42] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E453G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | The data suggest that some BCR-ABL1 mutations may persist at undetectable levels for many years after changing therapy, and can be reselected and confer resistance to subsequent inhibitors. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [42] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E275K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | The data suggest that some BCR-ABL1 mutations may persist at undetectable levels for many years after changing therapy, and can be reselected and confer resistance to subsequent inhibitors. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [29] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L340L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The frequency of ABL mutations in CML patients resistant to imatinib is high and is more frequent among those with clonal cytogenetic evolution. The change to second-generation TkI can overcome imatinib resistance in most of the mutated patients. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [29] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D276A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The frequency of ABL mutations in CML patients resistant to imatinib is high and is more frequent among those with clonal cytogenetic evolution. The change to second-generation TkI can overcome imatinib resistance in most of the mutated patients. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [24], [25], [26] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.I418V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The most frequent mutant is M244V, followed by Y253H, F359C/V/I, G250E, E255k, and T315I. Only seven patients (9%) have T315I mutants, and all showed hematologic resistance. Three of them were in the ECP and three in the LCP. Look-back studies show that mutants were detected 0-20 (median 7) months ahead of the appearance of clinical resistance in 15 tested patients with acquired resistance. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [32] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E453L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The most frequent mutant is M244V, followed by Y253H, F359C/V/I, G250E, E255k, and T315I. Only seven patients (9%) have T315I mutants, and all showed hematologic resistance. Three of them were in the ECP and three in the LCP. Look-back studies show that mutants were detected 0-20 (median 7) months ahead of the appearance of clinical resistance in 15 tested patients with acquired resistance. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [30], [32] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E450A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The most frequent mutant is M244V, followed by Y253H, F359C/V/I, G250E, E255k, and T315I. Only seven patients (9%) have T315I mutants, and all showed hematologic resistance. Three of them were in the ECP and three in the LCP. Look-back studies show that mutants were detected 0-20 (median 7) months ahead of the appearance of clinical resistance in 15 tested patients with acquired resistance. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [32] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E279Y |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | The most frequent mutant is M244V, followed by Y253H, F359C/V/I, G250E, E255k, and T315I. Only seven patients (9%) have T315I mutants, and all showed hematologic resistance. Three of them were in the ECP and three in the LCP. Look-back studies show that mutants were detected 0-20 (median 7) months ahead of the appearance of clinical resistance in 15 tested patients with acquired resistance. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15], [23], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.S417Y |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay | ||||||||||||
| Mechanism Description | We conclude that the currently recommended 10-fold threshold to trigger mutation screening is insensitive and not universally applicable. kinase domain mutations predict a shorter progression-free survival. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [15] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G251D |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay | ||||||||||||
| Mechanism Description | We conclude that the currently recommended 10-fold threshold to trigger mutation screening is insensitive and not universally applicable. kinase domain mutations predict a shorter progression-free survival. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F382L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay | ||||||||||||
| Mechanism Description | We conclude that the currently recommended 10-fold threshold to trigger mutation screening is insensitive and not universally applicable. kinase domain mutations predict a shorter progression-free survival. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26], [15] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E453K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay | ||||||||||||
| Mechanism Description | We conclude that the currently recommended 10-fold threshold to trigger mutation screening is insensitive and not universally applicable. kinase domain mutations predict a shorter progression-free survival. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [43] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.K419E |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirm the previously described poor prognosis of CML patients with mutations in the BCR-ABL1 kD, since 40.0% of our CML patients who harbored a BCR-ABL1 kD mutation died from CML while receiving TkI treatment. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [43] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E279K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirm the previously described poor prognosis of CML patients with mutations in the BCR-ABL1 kD, since 40.0% of our CML patients who harbored a BCR-ABL1 kD mutation died from CML while receiving TkI treatment. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [7] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.K294>RGG |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | BCR-ABL kinase domain mutations were sequentially analyzed in a patient with chronic myeloid leukemia (CML) who exhibited repeated B-lymphoid blast crisis (CML-BC) during treatment with imatinib and dasatinib. We first identified five mutant BCR-ABL clones: Y253H, G250E, F311L, F317L and k294RGG, which was generated by two-nucleotide mutations and six-nucleotide insertion, at the third BC during the imatinib treatment, and retrospectively found that three of them (Y253H, G250E, k294RGG) were already present at the second BC. | ||||||||||||
| Disease Class: Acute lymphocytic leukemia [ICD-11: 2B33.0] | [18] | ||||||||||||
| Resistant Disease | Acute lymphocytic leukemia [ICD-11: 2B33.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M244V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
CR-Abl sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay | ||||||||||||
| Mechanism Description | M244V and H396 mutations have been shown to be more resistant to imatinib but both have been shown to be sensitive to second generation TkI's such as nilotinib and dasatinib. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [36] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315N |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Denaturing high-power liquid chromatography assay | ||||||||||||
| Mechanism Description | Our results confirm the high frequency of BCR-ABL kinase domain mutations in patients with secondary resistance to imatinib and exclude mutations of the activation loops of kIT, PDGFRA and PDGFRB as possible causes of resistance in patients without ABL mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [36] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Denaturing high-power liquid chromatography assay | ||||||||||||
| Mechanism Description | Our results confirm the high frequency of BCR-ABL kinase domain mutations in patients with secondary resistance to imatinib and exclude mutations of the activation loops of kIT, PDGFRA and PDGFRB as possible causes of resistance in patients without ABL mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [19], [20], [21] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Allele-specific (AS)-RT-PCR assay | ||||||||||||
| Mechanism Description | We herein describe the development of a rapid allele-specific (AS)-RT-PCR assay to identify the T315I mutation, which confers full resistance to all available tyrosine-kinase inhibitors (TkI). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [44] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G398R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
Nested reverse transcriptase polymerase chain reaction assay; Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Two patients had p.E355G mutation in the catalytic domain, and the third patient had p.G398R in the activation loop that is reported here for the first time. Mutation status had no impact on the overall survival and progression-free survival. p.E355G mutation was correlated with shorter survival (P=0.047) in resistant patients. We conclude that BCR- ABL1 mutations are associated with the clinical resistance, but may not be considered the only cause of resistance to imatinib. Mutational analysis may identify resistant patients at risk of disease progression. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay; Allele-specific (AS)-RT-PCR assay | ||||||||||||
| Mechanism Description | We herein describe the development of a rapid allele-specific (AS)-RT-PCR assay to identify the T315I mutation, which confers full resistance to all available tyrosine-kinase inhibitors (TkI). | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Q252H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [15], [26] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M388L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [19], [20], [21] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M351T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M244V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [20], [21], [24] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.H396R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E459Q |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26], [31] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E355A |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [21], [24], [36] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26], [32], [40] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D276G |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [26], [34] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.A433T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vitro Model | Peripheral blood | Blood | Homo sapiens (Human) | N.A. | |||||||||
| Bone marrow | Blood | Homo sapiens (Human) | N.A. | ||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
cDNA sequencing assay; Standard dideoxy chain-termination DNA sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | Mutation scoring can predict outcome in CML-chronic phase with imatinib failure treated with second-generation TkIs and can help in therapy selection. | ||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.D444Y |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [14] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Imatinib | ||||||||||||
| Molecule Alteration | Expression | Up-regulation |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Cell Pathway Regulation | Cell apoptosis | Inhibition | hsa04210 | ||||||||||
| Cell proliferation | Activation | hsa05200 | |||||||||||
| In Vitro Model | K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |||||||||
| Ku812 cells | Bone marrow | Homo sapiens (Human) | CVCL_0379 | ||||||||||
| Experiment for Molecule Alteration |
Western blot analysis; qRT-PCR | ||||||||||||
| Experiment for Drug Resistance |
CCk reagent assay; Flow cytometry assay | ||||||||||||
| Mechanism Description | CircBA9.3 promoted cell proliferation and reduced the sensitivity of leukaemic cells to TkIs through up-regulation of the ABL1 and BCR-ABL1 protein expression levels. | ||||||||||||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [45] | |||
| Sensitive Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | |||
| Sensitive Drug | Imatinib | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Cell Pathway Regulation | BCR-ABL/PI3K/AKT signaling pathway | Inhibition | hsa05220 | |
| Cell apoptosis | Activation | hsa04210 | ||
| Cell proliferation | Inhibition | hsa05200 | ||
| In Vitro Model | K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 |
| Experiment for Molecule Alteration |
Western blot analysis; Dual luciferase reporter assay | |||
| Experiment for Drug Resistance |
CCK8 assay; Flow cytometric analysis | |||
| Mechanism Description | miR7 inhibits cell proliferation and increases cell apoptosis in k562 cells and downregulates BCR-ABL/PI3k/AkT signaling in k562 cells, thus sensitizing k562 cells to imatinib. | |||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [46] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | Our finding reflects the natural development of a T315I mutation within the hematopoietic system of the reported patient and indicates the importance of BCR-ABL1 mutation monitoring in more primitive cell populations. Considering the natural history of T315I development in this reported CML case, we hypothesize that BCR-ABL1 kD mutations may be pre-concentrated in more primitive CML cells, which subsequently expand into the PB. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [3], [10], [13] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.G250E |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Mutant Type Structure | Method: Solution NMR | Resolution: N.A. | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
60
|
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
-
R
-
70
|
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
-
G
-
80
|
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
-
K
-
90
|
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
-
N
-
100
|
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
-
D
-
110
|
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
-
S
-
120
|
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
-
L
-
130
|
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
-
E
-
140
|
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
-
V
-
150
|
P
-
S
-
N
-
Y
-
I
-
T
-
P
-
V
-
N
-
S
-
160
|
L
-
E
-
K
-
H
-
S
-
W
-
Y
-
H
-
G
-
P
-
170
|
V
-
S
-
R
-
N
-
A
-
A
-
E
-
Y
-
L
-
L
-
180
|
S
-
S
-
G
-
I
-
N
-
G
-
S
-
F
-
L
-
V
-
190
|
R
-
E
-
S
-
E
-
S
-
S
-
P
-
G
-
Q
-
R
-
200
|
S
-
I
-
S
-
L
-
R
-
Y
-
E
-
G
-
R
-
V
-
210
|
Y
-
H
-
Y
-
R
-
I
-
N
-
T
-
A
-
S
-
D
-
220
|
G
-
K
-
L
-
Y
-
V
-
S
-
S
-
E
-
S
-
R
-
230
|
F
-
N
-
T
-
L
-
A
-
E
-
L
-
V
-
H
-
H
-
240
|
H
-
S
-
T
-
V
-
A
-
D
-
G
-
L
-
I
-
T
-
250
|
T
-
L
-
H
-
Y
-
P
-
A
-
P
-
K
-
R
-
N
-
260
|
K
-
P
-
T
-
V
-
Y
-
G
-
V
-
S
S
P
P
N
N
270
|
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
D
D
280
|
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
E
G
G
290
|
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
W
W
300
|
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
K
K
310
|
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
E
E
320
|
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
L
K
K
330
|
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
L
L
340
|
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
F
F
350
|
Y
Y
I
I
I
I
I
T
E
E
F
F
M
M
T
T
Y
Y
G
G
360
|
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
N
N
370
|
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
L
L
380
|
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
M
M
390
|
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
H
H
400
|
R
R
N
D
L
L
A
A
A
A
R
R
N
N
C
C
L
L
V
V
410
|
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
D
D
420
|
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
Y
G
G
D
D
430
|
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
F
F
440
|
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
L
L
450
|
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
D
D
460
|
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
E
E
470
|
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
P
P
480
|
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
L
L
490
|
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
P
P
500
|
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
L
L
510
|
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
S
S
520
|
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
Q
Q
530
|
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
S
S
540
|
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
G
G
550
|
K
K
Q
Q
G
G
V
V
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
RNA sequencing assay | ||||||||||||
| Mechanism Description | The presence of BCR-ABL oncogene mutations in patients with chronic myeloid leukemia (CML) may be responsible for the failure of tyrosine kinase inhibitor (TkI) treatment. In addition to 9 point mutations (G250E / F317L, F359V, L387M, Y253H, M388L, M244V, T315I, D276G), 35 bp insertion between exons 8 and 9 and deletion exon 7 were detected. Our results demonstrate that direct sequencing is suitable for routine clinical monitoring patients with CML and may be useful for optimizing therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [47] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M351T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Progression-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | After 13 months of therapy a progression of disease to accelerated phase was detected and a second mutational screening analysis performed at that time revealed the absence of M244 V and the appearance of M351T mutation. After 14 months of therapy, a third mutational analysis was performed which revealed the disappearance of M351T mutation and the acquisition of a new F317L mutation. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [34] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359C |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Next generation sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | HSCT is an important salvage option for TkI-resistant patients with or without BCR-ABL1 mutations. Patients with mutations were more likely to develop advanced disease and had worse outcomes after HSCT. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [34] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Next generation sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | HSCT is an important salvage option for TkI-resistant patients with or without BCR-ABL1 mutations. Patients with mutations were more likely to develop advanced disease and had worse outcomes after HSCT. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [34] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.E255K |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Next generation sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Event-free survival assay; Overall survival assay | ||||||||||||
| Mechanism Description | HSCT is an important salvage option for TkI-resistant patients with or without BCR-ABL1 mutations. Patients with mutations were more likely to develop advanced disease and had worse outcomes after HSCT. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [10] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.F359I |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Mechanism Description | The most common mechanism of acquired resistance in CML in imatinib era is the acquisition of BCR-ABL kinase domain mutations with decreased sensitivity to the drug. Our findings demonstrate the potential hazards of sequential kinase inhibitor therapy and suggest a role for a combination of ABL kinase inhibitors, perhaps including drugs with different mechanisms of action, to prevent the outgrowth of cells harboring drug-resistant BCR-ABL mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L387M |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
RNA sequencing assay | ||||||||||||
| Mechanism Description | The presence of BCR-ABL oncogene mutations in patients with chronic myeloid leukemia (CML) may be responsible for the failure of tyrosine kinase inhibitor (TkI) treatment. In addition to 9 point mutations (G250E / F317L, F359V, L387M, Y253H, M388L, M244V, T315I, D276G), 35 bp insertion between exons 8 and 9 and deletion exon 7 were detected. Our results demonstrate that direct sequencing is suitable for routine clinical monitoring patients with CML and may be useful for optimizing therapy. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [13], [43] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Y253H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirm the previously described poor prognosis of CML patients with mutations in the BCR-ABL1 kD, since 40.0% of our CML patients who harbored a BCR-ABL1 kD mutation died from CML while receiving TkI treatment. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [43] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.H396R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirm the previously described poor prognosis of CML patients with mutations in the BCR-ABL1 kD, since 40.0% of our CML patients who harbored a BCR-ABL1 kD mutation died from CML while receiving TkI treatment. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [4] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Experiment for Drug Resistance |
Tritiated thymidine incorporation assay | ||||||||||||
| Mechanism Description | Mutations may impair TkI activity by directly or indirectly impairing the drug binding to the protein. We report the discovery of three new BCR/ABL mutations, L248R, T315V, and F317R identified in two patients with CML (L248R and T315V) and in one patient with Ph+ acute lymphoblastic leukemia (ALL) (F317R). | ||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [14] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Nilotinib | ||||||||||||
| Molecule Alteration | Expression | Up-regulation |
|||||||||||
| Experimental Note | Revealed Based on the Cell Line Data | ||||||||||||
| Cell Pathway Regulation | Cell apoptosis | Inhibition | hsa04210 | ||||||||||
| Cell proliferation | Activation | hsa05200 | |||||||||||
| In Vitro Model | K562 cells | Blood | Homo sapiens (Human) | CVCL_0004 | |||||||||
| Ku812 cells | Bone marrow | Homo sapiens (Human) | CVCL_0379 | ||||||||||
| Experiment for Molecule Alteration |
Western blot analysis; qRT-PCR | ||||||||||||
| Experiment for Drug Resistance |
CCk reagent assay; Flow cytometry assay | ||||||||||||
| Mechanism Description | CircBA9.3 promoted cell proliferation and reduced the sensitivity of leukaemic cells to TkIs through up-regulation of the ABL1 and BCR-ABL1 protein expression levels. | ||||||||||||
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Ponatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Ponatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.T212R |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Ponatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.Q252H |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Ponatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.M244V |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Ponatinib | ||||||||||||
| Molecule Alteration | Missense mutation | p.L387F |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Disease Class: Solid tumour/cancer [ICD-11: 2A00-2F9Z] | [5] | |||
| Sensitive Disease | Solid tumour/cancer [ICD-11: 2A00-2F9Z] | |||
| Sensitive Drug | Vandetanib | |||
| Molecule Alteration | Missense mutation | p.V299L (c.895G>C) |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Ba/F3 cells | Colon | Homo sapiens (Human) | CVCL_0161 |
| Ph+ALL cells | N.A. | N.A. | N.A. | |
| Mechanism Description | The missense mutation p.V299L (c.895G>C) in gene ABL1 cause the sensitivity of Vandetanib by aberration of the drug's therapeutic target | |||
Clinical Trial Drug(s)
1 drug(s) in total
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Disease Class: Solid tumour/cancer [ICD-11: 2A00-2F9Z] | [5] | |||
| Sensitive Disease | Solid tumour/cancer [ICD-11: 2A00-2F9Z] | |||
| Sensitive Drug | Foretinib | |||
| Molecule Alteration | Missense mutation | p.V299L (c.895G>C) |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Ba/F3 cells | Colon | Homo sapiens (Human) | CVCL_0161 |
| Ph+ALL cells | N.A. | N.A. | N.A. | |
| Mechanism Description | The missense mutation p.V299L (c.895G>C) in gene ABL1 cause the sensitivity of Foretinib by aberration of the drug's therapeutic target | |||
Investigative Drug(s)
1 drug(s) in total
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | |||||||||||||
|
|
|||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [49] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Tyrosine kinase inhibitor | ||||||||||||
| Molecule Alteration | Missense mutation | p.T315I |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.89 Å | |||||||||||
| Mutant Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
40
|
-
G
-
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
50
|
-
R
-
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
60
|
-
G
-
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
70
|
-
K
-
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
80
|
-
N
-
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
90
|
-
D
-
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
100
|
-
S
-
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
110
|
-
L
-
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
120
|
-
E
-
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
130
|
-
V
-
P
-
S
-
N
-
Y
M
I
A
T
S
P
V
V
N
N
140
|
S
S
L
L
E
E
K
K
H
H
S
S
W
W
Y
Y
H
H
G
G
150
|
P
P
V
V
S
S
R
R
N
N
A
A
A
A
E
E
Y
Y
L
L
160
|
L
L
S
S
S
S
G
G
I
I
N
N
G
G
S
S
F
F
L
L
170
|
V
V
R
R
E
E
S
S
E
E
S
S
S
S
P
P
G
G
Q
Q
180
|
R
R
S
S
I
I
S
S
L
L
R
R
Y
Y
E
E
G
G
R
R
190
|
V
V
Y
Y
H
H
Y
Y
R
R
I
I
N
N
T
T
A
A
S
S
200
|
D
D
G
G
K
K
L
L
Y
Y
V
V
S
S
S
S
E
E
S
S
210
|
R
R
F
F
N
N
T
T
L
L
A
A
E
E
L
L
V
V
H
H
220
|
H
H
H
H
S
S
T
T
V
V
A
A
D
D
G
G
L
L
I
I
230
|
T
T
T
T
L
L
H
H
Y
Y
P
P
A
A
P
P
K
K
R
R
240
|
N
N
K
K
P
P
T
T
V
V
Y
Y
G
G
V
V
S
S
P
P
250
|
N
N
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
260
|
D
D
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
G
270
|
G
G
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
280
|
W
W
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
290
|
K
K
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
300
|
E
E
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
M
310
|
K
K
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
320
|
L
L
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
330
|
F
F
Y
Y
I
I
I
I
T
I
E
E
F
F
M
M
T
T
Y
Y
340
|
G
G
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
350
|
N
N
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
360
|
L
L
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
370
|
M
M
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
380
|
H
H
R
R
D
N
L
L
A
A
A
A
R
R
N
N
C
C
L
L
390
|
V
V
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
400
|
D
D
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
T
G
G
410
|
D
D
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
420
|
F
F
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
430
|
L
L
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
440
|
D
D
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
450
|
E
E
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
460
|
P
P
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
470
|
L
L
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
480
|
P
P
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
490
|
L
L
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
500
|
S
S
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
510
|
Q
Q
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
520
|
S
S
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
530
|
G
G
K
K
Q
Q
G
G
V
V
L
-
E
-
H
-
H
-
H
-
540
|
H
-
H
-
H
-
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Mechanism Description | There are several identified mechanisms of resistance to TkIs. The presence of ABL kinase domain point mutation, which could be detected by molecular methods is one of them. ABL mutation was detected in 19 (31,6%) patients. In four cases with detected mutation the disease has progressed to blast crisis. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [49] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Tyrosine kinase inhibitor | ||||||||||||
| Molecule Alteration | Missense mutation | p.G250E |
|||||||||||
| Wild Type Structure | Method: X-ray diffraction | Resolution: 2.17 Å | |||||||||||
| Mutant Type Structure | Method: Solution NMR | Resolution: N.A. | |||||||||||
| Download The Information of Sequence | Download The Structure File | ||||||||||||
-
G
-
60
|
A
-
M
-
D
-
P
-
S
-
E
-
A
-
L
-
Q
-
R
-
70
|
P
-
V
-
A
-
S
-
D
-
F
-
E
-
P
-
Q
-
G
-
80
|
L
-
S
-
E
-
A
-
A
-
R
-
W
-
N
-
S
-
K
-
90
|
E
-
N
-
L
-
L
-
A
-
G
-
P
-
S
-
E
-
N
-
100
|
D
-
P
-
N
-
L
-
F
-
V
-
A
-
L
-
Y
-
D
-
110
|
F
-
V
-
A
-
S
-
G
-
D
-
N
-
T
-
L
-
S
-
120
|
I
-
T
-
K
-
G
-
E
-
K
-
L
-
R
-
V
-
L
-
130
|
G
-
Y
-
N
-
H
-
N
-
G
-
E
-
W
-
C
-
E
-
140
|
A
-
Q
-
T
-
K
-
N
-
G
-
Q
-
G
-
W
-
V
-
150
|
P
-
S
-
N
-
Y
-
I
-
T
-
P
-
V
-
N
-
S
-
160
|
L
-
E
-
K
-
H
-
S
-
W
-
Y
-
H
-
G
-
P
-
170
|
V
-
S
-
R
-
N
-
A
-
A
-
E
-
Y
-
L
-
L
-
180
|
S
-
S
-
G
-
I
-
N
-
G
-
S
-
F
-
L
-
V
-
190
|
R
-
E
-
S
-
E
-
S
-
S
-
P
-
G
-
Q
-
R
-
200
|
S
-
I
-
S
-
L
-
R
-
Y
-
E
-
G
-
R
-
V
-
210
|
Y
-
H
-
Y
-
R
-
I
-
N
-
T
-
A
-
S
-
D
-
220
|
G
-
K
-
L
-
Y
-
V
-
S
-
S
-
E
-
S
-
R
-
230
|
F
-
N
-
T
-
L
-
A
-
E
-
L
-
V
-
H
-
H
-
240
|
H
-
S
-
T
-
V
-
A
-
D
-
G
-
L
-
I
-
T
-
250
|
T
-
L
-
H
-
Y
-
P
-
A
-
P
-
K
-
R
-
N
-
260
|
K
-
P
-
T
-
V
-
Y
-
G
-
V
-
S
S
P
P
N
N
270
|
Y
Y
D
D
K
K
W
W
E
E
M
M
E
E
R
R
T
T
D
D
280
|
I
I
T
T
M
M
K
K
H
H
K
K
L
L
G
G
G
E
G
G
290
|
Q
Q
Y
Y
G
G
E
E
V
V
Y
Y
E
E
G
G
V
V
W
W
300
|
K
K
K
K
Y
Y
S
S
L
L
T
T
V
V
A
A
V
V
K
K
310
|
T
T
L
L
K
K
E
E
D
D
T
T
M
M
E
E
V
V
E
E
320
|
E
E
F
F
L
L
K
K
E
E
A
A
A
A
V
V
M
L
K
K
330
|
E
E
I
I
K
K
H
H
P
P
N
N
L
L
V
V
Q
Q
L
L
340
|
L
L
G
G
V
V
C
C
T
T
R
R
E
E
P
P
P
P
F
F
350
|
Y
Y
I
I
I
I
I
T
E
E
F
F
M
M
T
T
Y
Y
G
G
360
|
N
N
L
L
L
L
D
D
Y
Y
L
L
R
R
E
E
C
C
N
N
370
|
R
R
Q
Q
E
E
V
V
N
N
A
A
V
V
V
V
L
L
L
L
380
|
Y
Y
M
M
A
A
T
T
Q
Q
I
I
S
S
S
S
A
A
M
M
390
|
E
E
Y
Y
L
L
E
E
K
K
K
K
N
N
F
F
I
I
H
H
400
|
R
R
N
D
L
L
A
A
A
A
R
R
N
N
C
C
L
L
V
V
410
|
G
G
E
E
N
N
H
H
L
L
V
V
K
K
V
V
A
A
D
D
420
|
F
F
G
G
L
L
S
S
R
R
L
L
M
M
T
Y
G
G
D
D
430
|
T
T
Y
Y
T
T
A
A
H
H
A
A
G
G
A
A
K
K
F
F
440
|
P
P
I
I
K
K
W
W
T
T
A
A
P
P
E
E
S
S
L
L
450
|
A
A
Y
Y
N
N
K
K
F
F
S
S
I
I
K
K
S
S
D
D
460
|
V
V
W
W
A
A
F
F
G
G
V
V
L
L
L
L
W
W
E
E
470
|
I
I
A
A
T
T
Y
Y
G
G
M
M
S
S
P
P
Y
Y
P
P
480
|
G
G
I
I
D
D
L
L
S
S
Q
Q
V
V
Y
Y
E
E
L
L
490
|
L
L
E
E
K
K
D
D
Y
Y
R
R
M
M
E
E
R
R
P
P
500
|
E
E
G
G
C
C
P
P
E
E
K
K
V
V
Y
Y
E
E
L
L
510
|
M
M
R
R
A
A
C
C
W
W
Q
Q
W
W
N
N
P
P
S
S
520
|
D
D
R
R
P
P
S
S
F
F
A
A
E
E
I
I
H
H
Q
Q
530
|
A
A
F
F
E
E
T
T
M
M
F
F
Q
Q
E
E
S
S
S
S
540
|
I
I
S
S
D
D
E
E
V
V
E
E
K
K
E
E
L
L
G
G
550
|
K
K
Q
Q
G
G
V
V
|
|||||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| Mechanism Description | There are several identified mechanisms of resistance to TkIs. The presence of ABL kinase domain point mutation, which could be detected by molecular methods is one of them. ABL mutation was detected in 19 (31,6%) patients. In four cases with detected mutation the disease has progressed to blast crisis. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [48] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Tyrosine kinase inhibitor | ||||||||||||
| Molecule Alteration | Missense mutation | p.M351T |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Sanger sequencing assay | ||||||||||||
| Mechanism Description | Ponatinib was highly active in heavily pretreated patients with Ph-positive leukemias with resistance to tyrosine kinase inhibitors, including patients with the BCR-ABL T315I mutation, other mutations, or no mutations. | ||||||||||||
| Disease Class: Chronic myeloid leukemia [ICD-11: 2A20.0] | [6], [49] | ||||||||||||
| Resistant Disease | Chronic myeloid leukemia [ICD-11: 2A20.0] | ||||||||||||
| Resistant Drug | Tyrosine kinase inhibitor | ||||||||||||
| Molecule Alteration | Missense mutation | p.F317L |
|||||||||||
| Experimental Note | Identified from the Human Clinical Data | ||||||||||||
| In Vivo Model | A retrospective survey in conducting clinical studies | Homo sapiens | |||||||||||
| Experiment for Molecule Alteration |
Direct sequencing assay | ||||||||||||
| Mechanism Description | We confirmed the high frequency of SFks involvement in Tyrosine kinase inhibitor-resistant CML (52% of the cases) and even further in progressive disease and blast crises (60% of the cases). The SFks deregulation is also observed in patients harboring BCR-ABL mutations. In T315I and F317L mutated patients, CML-resistance appears to be promoted by SFks kinase protein reactivation once the BCR-ABL mutated clone has decreased on Omacetaxine. | ||||||||||||
Disease- and Tissue-specific Abundances of This Molecule
ICD Disease Classification 02

| Differential expression of molecule in resistant diseases | ||
| The Studied Tissue | Whole blood | |
| The Specified Disease | Myelofibrosis | |
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 8.68E-04; Fold-change: -2.63E-01; Z-score: -1.38E+00 | |
|
Molecule expression in the diseased tissue of patients
Molecule expression in the normal tissue of healthy individuals
|
||
| Disease-specific Molecule Abundances |

|
Click to View the Clearer Original Diagram |
| The Studied Tissue | Whole blood | |
| The Specified Disease | Polycythemia vera | |
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 8.73E-08; Fold-change: -1.77E-01; Z-score: -8.78E-01 | |
|
Molecule expression in the diseased tissue of patients
Molecule expression in the normal tissue of healthy individuals
|
||
| Disease-specific Molecule Abundances |

|
Click to View the Clearer Original Diagram |
| Differential expression of molecule in resistant diseases | ||
| The Studied Tissue | Lung | |
| The Specified Disease | Lung cancer | |
| The Expression Level of Disease Section Compare with the Healthy Individual Tissue | p-value: 1.79E-01; Fold-change: 2.11E-02; Z-score: 5.11E-02 | |
| The Expression Level of Disease Section Compare with the Adjacent Tissue | p-value: 3.53E-09; Fold-change: -4.31E-01; Z-score: -7.79E-01 | |
|
Molecule expression in the normal tissue adjacent to the diseased tissue of patients
Molecule expression in the diseased tissue of patients
Molecule expression in the normal tissue of healthy individuals
|
||
| Disease-specific Molecule Abundances |

|
Click to View the Clearer Original Diagram |
Tissue-specific Molecule Abundances in Healthy Individuals

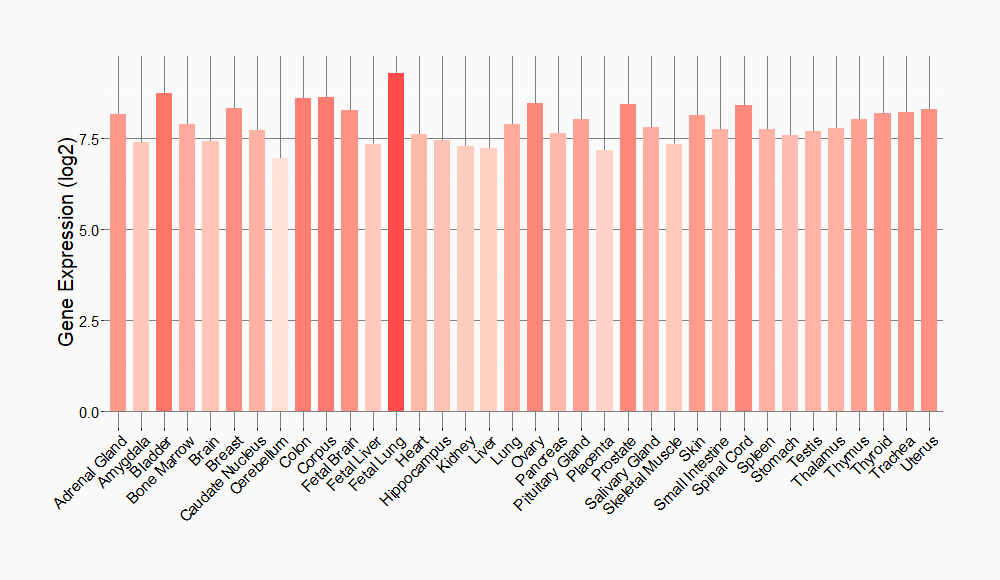
|
||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
