Drug Information
Drug (ID: DG00681) and It's Reported Resistant Information
| Name |
Pyrazinamide
|
||||
|---|---|---|---|---|---|
| Synonyms |
Pyrazinamide; pyrazinecarboxamide; 98-96-4; pyrazine-2-carboxamide; pyrazinoic acid amide; Zinamide; 2-Pyrazinecarboxamide; Aldinamide; Aldinamid; Pirazinamid; Tebrazid; Farmizina; Pirazimida; Pyrazineamide; Unipyranamide; Eprazin; Novamid; Pyrafat; pyrazine carboxylamide; 2-Carbamylpyrazine; Pyrazinecarboxylic acid amide; Pyrazinamidum; Isopas; Pirazinamide; Pyrazine carboxamide; D-50; MK 56; C5H5N3O; PZA; NCI-C01785; UNII-2KNI5N06TI; MFCD00006132; NSC 14911; T 165; Pirazinamida; Tisamid; 2KNI5N06TI; MLS000069730; Pezetamid; Piraldina; Pyrazide; CHEBI:45285; Rozide; NSC14911; Pyrazinamide (Pyrazinoic acid amide); NSC-14911; NCGC00015833-09; Pyrazinamdie; SMR000036662; Pirazinamide [DCIT]; DSSTox_CID_1215; DSSTox_RID_76014; DSSTox_GSID_21215; Pyrazinamidum [INN-Latin]; Pirazinamida [INN-Spanish]; pyramizade; Rifafour; D-50 (VAN); DRG 0124; CAS-98-96-4; CCRIS 545; Pyrazinamide (TN); Rifafour e-200; HSDB 3576; SR-01000076077; EINECS 202-717-6; BRN 0112306; pyrazinamida; Pyrizinamide; pyrazine amide; AZT + Pyrazinamide combination; Pyrazine-2-carboxylic acid amide; Pyrazinamide,(S); Pyrazinamide [USP:INN:BAN:JAN]; Prestwick_811; .alpha.-pyrazinamide; 2-pyrazine carboxamide; Spectrum_000902; Opera_ID_735; Prestwick0_000514; Prestwick1_000514; Prestwick2_000514; Prestwick3_000514; Spectrum2_001305; Spectrum3_001046; Spectrum4_001186; Spectrum5_001026; Lopac-P-7136; CHEMBL614; P 7136; WLN: T6N DNJ BVZ; pyrazine-2-carboximidic acid; Lopac0_001011; SCHEMBL24102; BSPBio_000467; BSPBio_002572; KBioGR_001851; KBioSS_001382; 5-25-04-00178 (Beilstein Handbook Reference); MLS002222347; BIDD:GT0228; DivK1c_000241; SPECTRUM1500518; SPBio_001369; SPBio_002388; BPBio1_000515; GTPL7287; ZINC2005; DTXSID9021215; HMS500M03; KBio1_000241; KBio2_001382; KBio2_003950; KBio2_006518; KBio3_001792; Pyrazinamide (JP17/USP/INN); NINDS_000241; BDBM228814; HMS1569H09; HMS1920N08; HMS2092E09; HMS2096H09; HMS2235G17; HMS3259O04; HMS3263K03; HMS3371G09; HMS3655A10; HMS3713H09; KUC109577N; Pharmakon1600-01500518; ACT01761; AMY14180; BCP30257; HY-B0271; KSC-27-052E; Pyrazine-[d3]-carboxamide-[15N]; Tox21_110237; Tox21_202059; Tox21_302771; Tox21_501011; CCG-39243; NSC757304; s1762; STK801661; AKOS000120280; Tox21_110237_1; DB00339; LP01011; MCULE-6846697749; NC00534; NSC-757304; Pyrazinecarboxamide, analytical standard; SDCCGSBI-0050984.P005; IDI1_000241; NCGC00015833-01; NCGC00015833-02; NCGC00015833-03; NCGC00015833-04; NCGC00015833-05; NCGC00015833-06; NCGC00015833-07; NCGC00015833-08; NCGC00015833-10; NCGC00015833-11; NCGC00015833-12; NCGC00015833-15; NCGC00015833-16; NCGC00015833-25; NCGC00090695-01; NCGC00090695-03; NCGC00090695-04; NCGC00090695-05; NCGC00090695-06; NCGC00090695-07; NCGC00256336-01; NCGC00259608-01; NCGC00261696-01; Pyrazinoic acid amide; pyrazinamide; PZA; CAS- 98-96-4; SY013550; TS-01626; SBI-0050984.P004; DB-002866; AB00052083; B2122; BB 0253141; EU-0101011; FT-0659757; P0633; SW196945-3; C01956; D00144; D70481; J10111; 1,2-dihydro-1,2,4-triazol-3-one;Pyrazinamide; AB00052083-16; AB00052083_17; AB00052083_18; A845937; AC-907/25014068; Q417571; SR-01000076077-1; SR-01000076077-4; SR-01000076077-6; W-100059; Z33546644; Pyrazinamide, British Pharmacopoeia (BP) Reference Standard; Pyrazinamide, European Pharmacopoeia (EP) Reference Standard; 2-Carbamylpyrazine ;Aldinamid ;Aldinamide; Pyrazinoic acid amide; Pyrazinamide, United States Pharmacopeia (USP) Reference Standard; Pyrazinamide, Pharmaceutical Secondary Standard; Certified Reference Material
Click to Show/Hide
|
||||
| Indication |
In total 1 Indication(s)
|
||||
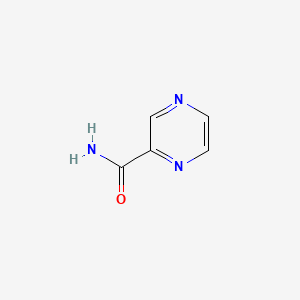
| Structure |
|
||||
| Drug Resistance Disease(s) |
Disease(s) with Resistance Information Discovered by Cell Line Test for This Drug
(2 diseases)
[2]
[3]
Disease(s) with Clinically Reported Resistance for This Drug
(2 diseases)
[1]
[4]
|
||||
| Target | Bacterial Fatty acid synthetase I (Bact inhA) | INHA_MYCTU | [1] | ||
| Click to Show/Hide the Molecular Information and External Link(s) of This Drug | |||||
| Formula |
C5H5N3O
|
||||
| IsoSMILES |
C1=CN=C(C=N1)C(=O)N
|
||||
| InChI |
1S/C5H5N3O/c6-5(9)4-3-7-1-2-8-4/h1-3H,(H2,6,9)
|
||||
| InChIKey |
IPEHBUMCGVEMRF-UHFFFAOYSA-N
|
||||
| PubChem CID | |||||
| ChEBI ID | |||||
| TTD Drug ID | |||||
| INTEDE ID | |||||
| DrugBank ID | |||||
Type(s) of Resistant Mechanism of This Drug
Drug Resistance Data Categorized by Their Corresponding Diseases
ICD-01: Infectious/parasitic diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Pyrazinamidase/nicotinamidase (PncA) | [3] | |||
| Resistant Disease | Tuberculosis [ICD-11: 1B10.0] | |||
| Molecule Alteration | Mutation | Q859H/K |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Experiment for Molecule Alteration |
GeneSeq assay; Bioinformatics assay | |||
| Mechanism Description | Out of total 112 mycobacterial positive cultures, five?M. bovis?were isolated and underwent WGS. All sequenced strains belonged to?Mycobacterium tuberculosis var bovis, spoligotype BOV_1; BOV_11. Resistance gene mutations were determined in 100% of strains to pyrazinamide (pncA?and?rpsA), isoniazid (KatG?and?ahpC), ethambutol (embB,?embC,?embR?and?ubiA), streptomycin (rpsl) and fluoroquinolones (gyrA?and?gyrB). Rifampin (rpoB?and?rpoC) and delamanid (fbiC) resistance genes were found in 80% of strains. The major represented virulence classes were the secretion system, cell surface components and regulation system. | |||
| Key Molecule: Small ribosomal subunit protein uS2 (RPSA) | [3] | |||
| Resistant Disease | Tuberculosis [ICD-11: 1B10.0] | |||
| Molecule Alteration | Mutation | rpoB gene |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| Experiment for Molecule Alteration |
GeneSeq assay; Bioinformatics assay | |||
| Mechanism Description | Out of total 112 mycobacterial positive cultures, five?M. bovis?were isolated and underwent WGS. All sequenced strains belonged to?Mycobacterium tuberculosis var bovis, spoligotype BOV_1; BOV_11. Resistance gene mutations were determined in 100% of strains to pyrazinamide (pncA?and?rpsA), isoniazid (KatG?and?ahpC), ethambutol (embB,?embC,?embR?and?ubiA), streptomycin (rpsl) and fluoroquinolones (gyrA?and?gyrB). Rifampin (rpoB?and?rpoC) and delamanid (fbiC) resistance genes were found in 80% of strains. The major represented virulence classes were the secretion system, cell surface components and regulation system. | |||
ICD-X: Extension Codes
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Pyrazinamidase | [2] | |||
| Resistant Disease | bifidobacterium adolescentis infection [ICD-11: XN33F] | |||
| Molecule Alteration | Missense mutation | Q24K+L28M+R30E+A92K |
||
| Experimental Note | Revealed Based on the Cell Line Data | |||
| In Vitro Model | Bifidobacterial strains | 1763 | ||
| Experiment for Molecule Alteration |
PCR; Catalase foam assay; Catalase gel assay | |||
| Experiment for Drug Resistance |
Growth curve assay; Spot assay; Anti-tubercular drug uptake and surface assay; Adaptability assay; FE-SEM assay; MIC assay; Particle size assay | |||
| Mechanism Description | The current study aims to understand the resistance of Bifidobacterium adolescentis to different anti-tubercular drugs (first-line oral tuberculosis drugs). The bacteria were grown with anti-tubercular drugs such as isoniazid, pyrazinamide, and streptomycin to better understand the resistance phenomena. It was found that even at tenfold higher concentrations, growth rates remained unchanged. In addition, a small number of bacteria were found to aggregate strongly, a property that protects against the toxicity of the drug. Further FE-SEM (Field Emission Scanning Electron Microscopy) analysis revealed that some bacteria became excessively long, elongated, and protruded on the surface. Size scattering analysis confirmed the presence of bifidobacteria in the size range of 1.0-100 um. After whole genome sequence analysis, certain mutations were found in the relevant gene. In vitro, foam formation and growth in the presence of H2O2 and HPLC (High Performance Liquid Chromatography) studies provide additional evidence for the presence of catalase. According to RAST (Rapid Annotation Using Subsystems Technology) annotation and CARD (Comprehensive Antibiotic Resistance Database analysis), there were not many components in the genome that were resistant to antibiotics. Whole genome sequence (WGS) analysis does not show the presence of bacteriocins and antibiotic resistance genes, but few hypothetical proteins were observed. 3D structure and docking studies suggest their interaction with specific ligands. | |||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
