Drug Information
Drug (ID: DG00551) and It's Reported Resistant Information
| Name |
Leflunomide
|
||||
|---|---|---|---|---|---|
| Synonyms |
Leflunomide; 75706-12-6; Arava; lefunamide; Leflunomida; Leflunomidum; 5-methyl-N-[4-(trifluoromethyl)phenyl]-1,2-oxazole-4-carboxamide; HWA 486; Leflunomidum [INN-Latin]; HWA-486; Repso; SU101; Arava (TN); 5-methyl-N-(4-(trifluoromethyl)phenyl)isoxazole-4-carboxamide; 5-Methyl-N-(4-(trifluoromethyl)phenyl)-4-isoxazolecarboxamide; 5-Methylisoxazole-4-carboxylic acid (4-trifluoromethyl)anilide; 4-Isoxazolecarboxamide, 5-methyl-N-[4-(trifluoromethyl)phenyl]-; alpha,alpha,alpha-Trifluoro-5-methyl-4-isoxazolecarboxy-p-toluidide; UNII-G162GK9U4W; SU-101; 5-methyl-N-[4-(trifluoromethyl)phenyl]isoxazole-4-carboxamide; RS-34821; CHEMBL960; MLS000069648; CHEBI:6402; G162GK9U4W; 5-Methylisoxazole-4-(4-trifluoromethylcarboxanilide); MFCD00867593; NSC-677411; NSC-759864; NCGC00015610-02; SMR000058209; 5-methyl-N-[4-(trifluoromethyl)phenyl]-4-isoxazolecarboxamide; 4-Isoxazolecarboxamide, 5-methyl-N-(4-(trifluoromethyl)phenyl)-; CAS-75706-12-6; leflunomide medac; DSSTox_CID_3201; DSSTox_RID_76923; DSSTox_GSID_23201; Leflunomida [INN-Spanish]; SU 101 (pharmaceutical); Lefunomide [Inn-Spanish]; HSDB 7289; SR-01000000191; Arabloc; HWA486; Leflunomide teva; N-(4'-Trifluoromethylphenyl)-5-methylisoxazole-4-carboxamide; L04AA13; Prestwick_87; Leflunomide [USAN:USP:INN:BAN]; Leflunomide winthrop; SU 101; SULOL; Leflunomide ratiopharm; Spectrum_000322; Opera_ID_1709; Prestwick0_000772; Prestwick1_000772; Prestwick2_000772; Prestwick3_000772; Spectrum5_000850; Lopac-L-5025; L 5025; SCHEMBL5057; BIDD:PXR0189; Lopac0_000649; BSPBio_000844; KBioSS_000802; Leflunomide, Immunosuppressant; MLS001076267; DivK1c_000916; Leflunomide (JAN/USP/INN); SPECTRUM1503927; 5-Methylisoxazole-4-(4-trifluoromethyl)carboxanilide; SPBio_002783; BPBio1_000930; GTPL6825; ZINC4840; DTXSID9023201; HMS502N18; KBio1_000916; KBio2_000802; KBio2_003370; KBio2_005938; AOB5964; NINDS_000916; 4-Isoxazolecarboxamide, 5-methyl-N-(4-(trifluoromethyl)phenyl; HMS1570K06; HMS1922M06; HMS2090O12; HMS2097K06; HMS2235C07; HMS3262A19; HMS3268D12; HMS3371F21; HMS3414P03; HMS3654F07; HMS3673M17; HMS3678N21; HMS3714K06; HMS3865I13; Pharmakon1600-01503927; ALBB-019233; BCP22241; HY-B0083; Tox21_110182; Tox21_301873; Tox21_500649; BDBM50054601; DL-433; NSC677411; NSC759864; s1247; STL426823; AKOS000265193; Tox21_110182_1; AC-6796; BCP9000846; CCG-204736; CS-1781; DB01097; KS-1076; LP00649; MCULE-9490869974; NSC 677411; NSC 759864; SB17287; SDCCGSBI-0050629.P003; IDI1_000916; NCGC00015610-01; NCGC00015610-03; NCGC00015610-04; NCGC00015610-05; NCGC00015610-06; NCGC00015610-07; NCGC00015610-08; NCGC00015610-09; NCGC00015610-10; NCGC00015610-11; NCGC00015610-12; NCGC00015610-13; NCGC00015610-14; NCGC00015610-17; NCGC00015610-18; NCGC00015610-30; NCGC00022625-03; NCGC00022625-04; NCGC00022625-05; NCGC00022625-06; NCGC00022625-07; NCGC00022625-08; NCGC00255370-01; NCGC00261334-01; BM164612; H527; Leflunomide 100 microg/mL in Acetonitrile; A9622; AB00052389; EU-0100649; FT-0621959; L0250; SW196399-3; C07905; D00749; MLS-0003109.0001; AB00052389-17; AB00052389-18; AB00052389_19; AB00052389_21; 706L126; Q248550; Q-201289; SR-01000000191-2; SR-01000000191-4; SR-01000000191-7; BRD-K78692225-001-03-9; BRD-K78692225-001-11-2; 5-methyl-4-(4-trifluoromethyl-phenyl)aminocarbonylisoxazole; 5-methyl-4-(4-trifluoromethylphenyl)aminocarbonylisoxazole; Leflunomide, European Pharmacopoeia (EP) Reference Standard; N-(4-trifluoromethylphenyl)-5-methylisoxazole-4-carboxamide; 5-Methyl-N-[4-(trifluoromethyl)-phenyl]isoxazole-4-carboxamide; 5-methylisoxazole-4-carboxylic acid (4-trifluoromethyl)-anilide; N-(4-trifluoromethylphenyl)-5-methylisoxa-zole-4-carboxamide; Isoxazole-4-carboxamide, 5-methyl-N-[4-(trifluoromethyl)phenyl]-; Leflunomide, United States Pharmacopeia (USP) Reference Standard; 5-methyl-N-(4-(trifluoromethyl)phenyl)isoxazole-4-carboxamide;Leflunomide; HWA486; RS-34821; SU101;HWA 486; RS 34821; SU 101; Leflunomide, Pharmaceutical Secondary Standard; Certified Reference Material; Leflunomide for peak identification, European Pharmacopoeia (EP) Reference Standard
Click to Show/Hide
|
||||
| Indication |
In total 2 Indication(s)
|
||||
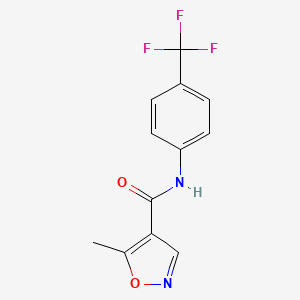
| Structure |
|
||||
| Drug Resistance Disease(s) |
Disease(s) with Clinically Reported Resistance for This Drug
(1 diseases)
[1]
|
||||
| Target | Plasmodium Dihydroorotate dehydrogenase (Malaria DHOdehase) | PYRD_PLAF7 | [1] | ||
| Click to Show/Hide the Molecular Information and External Link(s) of This Drug | |||||
| Formula |
C12H9F3N2O2
|
||||
| IsoSMILES |
CC1=C(C=NO1)C(=O)NC2=CC=C(C=C2)C(F)(F)F
|
||||
| InChI |
1S/C12H9F3N2O2/c1-7-10(6-16-19-7)11(18)17-9-4-2-8(3-5-9)12(13,14)15/h2-6H,1H3,(H,17,18)
|
||||
| InChIKey |
VHOGYURTWQBHIL-UHFFFAOYSA-N
|
||||
| PubChem CID | |||||
| ChEBI ID | |||||
| TTD Drug ID | |||||
| VARIDT ID | |||||
| INTEDE ID | |||||
| DrugBank ID | |||||
Type(s) of Resistant Mechanism of This Drug
Drug Resistance Data Categorized by Their Corresponding Diseases
ICD-02: Benign/in-situ/malignant neoplasm
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Dihydroorotate dehydrogenase (DHODH) | [2] | |||
| Sensitive Disease | Cholangiocarcinoma [ICD-11: 2C12.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | Mitochondrial ferroptosis regulatory signaling pathway | Regulation | N.A. | |
| In Vivo Model | Mouse model | Mus musculus | ||
| Experiment for Molecule Alteration |
Immunoprecipitation assay; LC-MS/MS analysis | |||
| Experiment for Drug Resistance |
Cellular ROS and lipid peroxidation level assay; LOXL3 enzymatic assay; In vitro kinase assay | |||
| Mechanism Description | To overcome chemotherapy resistance, novel strategies sensitizing cancer cells to chemotherapy are required. Here, we screen the lysyl-oxidase (LOX) family to clarify its contribution to chemotherapy resistance in liver cancer. LOXL3 depletion significantly sensitizes liver cancer cells to Oxaliplatin by inducing ferroptosis. Chemotherapy-activated EGFR signaling drives LOXL3 to interact with TOM20, causing it to be hijacked into mitochondria, where LOXL3 lysyl-oxidase activity is reinforced by phosphorylation at S704. Metabolic adenylate kinase 2 (AK2) directly phosphorylates LOXL3-S704. Phosphorylated LOXL3-S704 targets dihydroorotate dehydrogenase (DHODH) and stabilizes it by preventing its ubiquitin-mediated proteasomal degradation. K344-deubiquitinated DHODH accumulates in mitochondria, in turn inhibiting chemotherapy-induced mitochondrial ferroptosis. CRISPR-Cas9-mediated site-mutation of mouse LOXL3-S704 to D704 causes a reduction in lipid peroxidation. Using an advanced liver cancer mouse model, we further reveal that low-dose Oxaliplatin in combination with the DHODH-inhibitor Leflunomide effectively inhibit liver cancer progression by inducing ferroptosis, with increased chemotherapy sensitivity and decreased chemotherapy toxicity. | |||
ICD-15: Musculoskeletal/connective-tissue diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: ATP-binding cassette sub-family G2 (ABCG2) | [1] | |||
| Resistant Disease | Rheumatoid arthritis [ICD-11: FA20.0] | |||
| Molecule Alteration | Expression | Up-regulation |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | MTX is a substrate for eight ABC transporters. In vitro studies demonstrated that RAFLS treated with MTX had higher ABCB1 expression levels than controls, with a positive correlation between ABCB1 expression levels and RA treatment duration. In addition to MTX, other DMARDs (e.g. sulfasalazine, leflunomide, bucillamine, azathioprine), glucocorticoids (e.g. betamethasone, dexamethasone), and NSAIDs (e.g. celecoxib and indomethacin) are also substrates of ABC transporters. | |||
|
|
||||
| Key Molecule: Cellular tumor antigen p53 (TP53) | [1] | |||
| Resistant Disease | Rheumatoid arthritis [ICD-11: FA20.0] | |||
| Molecule Alteration | Mutation | p.P151S+p.R175H+p.G245C+p.R282W |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | The wild-type p53 tumor suppressor (p53) is overexpressed in response to DNA damage and inflammation in RA fibroblast-like synoviocytes (FLS), which are highly specialized mesenchymal cells located in the internal lining of the synovium and are involved in the pathogenesis and progression of RA. In line with the effects of p53 gain-of-function mutation in tumor progression, mutation-mediated gain-of-function of p53 may contribute to the invasiveness and apoptosis-resistant feature of FLS in RA and the increased expression of cartilage degradative proteases, leading to degeneration of cartilage and bone. Gene knockout or gene transfer studies using a collagen-II-induced arthritis (CIA) model have established the crucial role of p53 in RA that provides a basis for additional research to fully characterize the clinical implications of p53 somatic mutations in drug-resistant RA. | |||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
