Drug Information
Drug (ID: DG00633) and It's Reported Resistant Information
| Name |
Diclofenac
|
||||
|---|---|---|---|---|---|
| Synonyms |
Diclofenac; 15307-86-5; Diclofenac acid; dichlofenac; Diclofenacum; Diclophenac; 2-(2-((2,6-Dichlorophenyl)amino)phenyl)acetic acid; Diclofenaco; Diclofenac resinate; Voltarol; 2-(2,6-Dichloroanilino)phenylacetic Acid; 2-[2-(2,6-dichloroanilino)phenyl]acetic acid; 2-{2-[(2,6-dichlorophenyl)amino]phenyl}acetic acid; Benzeneacetic acid, 2-[(2,6-dichlorophenyl)amino]-; 2-((2,6-Dichlorophenyl)amino)benzeneacetic acid; Solaraze; Diclofenac free acid; UNII-144O8QL0L1; {2-[(2,6-dichlorophenyl)amino]phenyl}acetic acid; CHEBI:47381; Voltaren-XR; [2-(2,6-Dichloroanilino)phenyl]acetic acid; 2-[(2,6-Dichlorophenyl)amino]benzeneacetic acid; CHEMBL139; 2-[2,6-DICHLOROPHENYL)AMINO]BENZENEACETIC ACID; ACETIC ACID, (o-(2,6-DICHLOROANILINO)PHENYL)-; 144O8QL0L1; Arthrotec; 15307-86-5 (free); ProSorb-D; Olfen; MFCD00056694; Solaraze (TN); 2-[(2,6-dichlorophenyl)amino]-benzeneacetic acid; Enfenamic acid; N-Phenethylanthranilic acid; RH 8; 2-[2-[(2,6-dichlorophenyl)amino]phenyl]acetic acid; Zorovolex; Zorvolex; Diclofenamic acid; Diclofenacum [INN-Latin]; Diclofenaco [INN-Spanish]; DIF; HSDB 7234; GP-45840; EINECS 239-348-5; (2-((2,6-Dichlorophenyl)amino-phenyl)acetic acid (HD); BRN 2146636; Diclofenac [USAN:INN:BAN]; ISV-205; Zorvolex (TN); Spectrum_000930; Diclofenac (USAN/INN); Prestwick0_000594; Prestwick1_000594; Prestwick2_000594; Prestwick3_000594; Spectrum2_000991; Spectrum3_000385; Spectrum4_000506; Spectrum5_000867; Epitope ID:116873; EC 239-348-5; SCHEMBL2799; Lopac0_000441; Oprea1_011155; BSPBio_000468; BSPBio_002169; KBioGR_001051; KBioGR_002306; KBioSS_001410; KBioSS_002308; MLS006011795; BIDD:GT0380; DivK1c_000272; DivK1c_000402; 2-[2-(2,6-dichlorophenyl)aminophenyl]ethanoic acid; SPBio_001081; SPBio_002687; BPBio1_000516; GTPL2714; ZINC1281; DTXSID6022923; BDBM13066; HMS501E04; KBio1_000272; KBio1_000402; KBio2_001410; KBio2_002306; KBio2_003978; KBio2_004874; KBio2_006546; KBio2_007442; KBio3_001389; KBio3_002786; 2b17; cMAP_000014; NINDS_000272; NINDS_000402; HMS2090C10; HMS3886F09; BCP09087; BCP13860; LAS41007; LAS-41007; s6073; STK984493; AKOS001579542; DB00586; KS-1258; MCULE-1824024270; IDI1_000272; IDI1_000402; NCGC00021125-01; NCGC00021125-02; NCGC00021125-11; AC-27673; HY-15036; o-(2,6-dichloroanilino)phenylacetic acid; SMR001550371; SY038623; SBI-0051341.P003; D3748; FT-0624731; FT-0666643; UNM000001216103; [2-(2,6-Dichloroanilino)phenyl]acetic acid #; C01690; D07816; Diclofenac acid 100 microg/mL in Acetonitrile; H10425; [o-(2,6-dichloro-anilino)-phenyl]-acetic acid; 2-[(2,6-dichlorophenyl)amino]phenylacetic acid; 2-[2-(2,6-dichloroanilino)phenyl]acetic acid.; AB01275502-01; AB01275502_02; 056D694; 2-(2-(2,6-dichlorophenylamino)phenyl)acetic acid; 2-[(2,6-dichlorophenyl)amino]-phenyl-acetic acid; Q244408; [2-(2,6-dichloro-phenylamino)-phenyl]-acetic acid; 2-[(2,6-dichlorophenyl)-amino]-benzeneacetic acid; 2-[(2,6-dichlorophenyl)-amino]-phenyl-acetic acid; 2-[2-(2,6-dichlorophenylamino)phenyl]-acetic acid; SR-01000003041-3; 2-[2-(2,6-dichlorophenylamino)-phenyl]-acetic acid; BRD-K08252256-236-05-6; BRD-K08252256-236-17-1; Z57664869; F0722-0745; Benzeneacetic acid, 2-((2,6-dichlorophenyl)amino)- (9CI); 2-[2-[(2,6-Dichlorophenyl)amino]phenyl]acetic Acid (Diclofenac); 128402-48-2
Click to Show/Hide
|
||||
| Indication |
In total 1 Indication(s)
|
||||
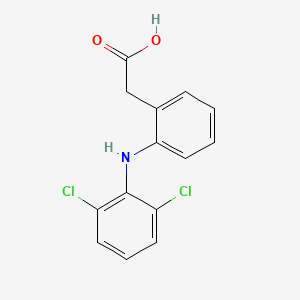
| Structure |
|
||||
| Drug Resistance Disease(s) |
Disease(s) with Clinically Reported Resistance for This Drug
(1 diseases)
[1]
|
||||
| Target | Prostaglandin G/H synthase (COX) |
PGH1_HUMAN
; PGH2_HUMAN |
[2] | ||
| Click to Show/Hide the Molecular Information and External Link(s) of This Drug | |||||
| Formula |
C14H11Cl2NO2
|
||||
| IsoSMILES |
C1=CC=C(C(=C1)CC(=O)O)NC2=C(C=CC=C2Cl)Cl
|
||||
| InChI |
1S/C14H11Cl2NO2/c15-10-5-3-6-11(16)14(10)17-12-7-2-1-4-9(12)8-13(18)19/h1-7,17H,8H2,(H,18,19)
|
||||
| InChIKey |
DCOPUUMXTXDBNB-UHFFFAOYSA-N
|
||||
| PubChem CID | |||||
| ChEBI ID | |||||
| TTD Drug ID | |||||
| VARIDT ID | |||||
| DrugBank ID | |||||
Type(s) of Resistant Mechanism of This Drug
Drug Resistance Data Categorized by Their Corresponding Diseases
ICD-01: Infectious/parasitic diseases
| Drug Sensitivity Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Beta-lactam-inducible penicillin-binding protein (MECA) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
|
|
||||
| Key Molecule: Autolysins enzymes (ALTE) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: Beta-lactamase (BLAC) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: Aminoacyltransferase FemA (FEMA) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: Aminoacyltransferase FemB (FEMB) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: Formin binding protein 1 (FNBP1) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: Mitochondrial trans-2-enoyl-CoA reductase (MECR) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: UDP-N-acetylglucosamine 1-carboxyvinyltransferase 1 (MURA1) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
| Key Molecule: UDP-N-acetylmuramate-L-alanine ligase (MURC) | [2] | |||
| Sensitive Disease | Staphylococcus aureus infection [ICD-11: 1B54.0] | |||
| Molecule Alteration | Expression | Down-regulation |
||
| Experimental Note | Discovered Using In-vivo Testing Model | |||
| Cell Pathway Regulation | mecA/blaZ pathway | Activation | hsa01501 | |
| In Vivo Model | Murine skin and soft tissue infection model | Mus musculus | ||
| Experiment for Molecule Alteration |
Gene expression analysis; Cellular ATP level assay; Ethidium bromide efflux inhibition assay | |||
| Experiment for Drug Resistance |
CCK-8 assay | |||
| Mechanism Description | High-dose diclofenac can inhibit the growth of MRSA, and does not easily induce drug-resistant mutations after continuous passage. Low-doses diclofenac can resensitize bacteria to beta-lactams, which help to circumvent drug resistance and improve the antibacterial efficacy of conventional antibiotics. Diclofenac can reduce the expression of genes and proteins associated with beta-lactam resistance, low dose diclofenac can inhibit MRSA antibiotic resistance via the mecA/blaZ pathway and related biofilms in implants. | |||
ICD-16: Genitourinary system diseases
| Drug Resistance Data Categorized by Their Corresponding Mechanisms | ||||
|
|
||||
| Key Molecule: Cytochrome P450 family 2 subfamily C member 9 (CYP2C9) | [1] | |||
| Resistant Disease | Dysmenorrhea [ICD-11: GA34.3] | |||
| Molecule Alteration | SNP | CYP2C9*2/*2 |
||
| Experimental Note | Identified from the Human Clinical Data | |||
| Mechanism Description | For example, the CYP2C9*2/*2 polymorphism was associated with increased total clearance of celecoxib and diclofenac.48 More research is necessary to determine if other gain-of-function variants exist and alter NSAID metabolism. | |||
References
If you find any error in data or bug in web service, please kindly report it to Dr. Sun and Dr. Yu.
